For many women, having a regular menstrual cycle is seen as a sign of reproductive health. However, it’s entirely possible—and more common than you might think—to experience what appears to be a normal period without actually ovulating. This phenomenon, known as an anovulatory cycle, can be confusing and concerning, especially for those trying to conceive or simply seeking to understand their bodies better.
In this comprehensive guide, we’ll explore the science behind anovulatory cycles, explain why they occur, and discuss how they can still result in what looks like a regular period. We’ll also cover diagnostic methods, potential underlying health conditions, and practical steps you can take to support your reproductive health.
What Is Ovulation—and Why Does It Matter?
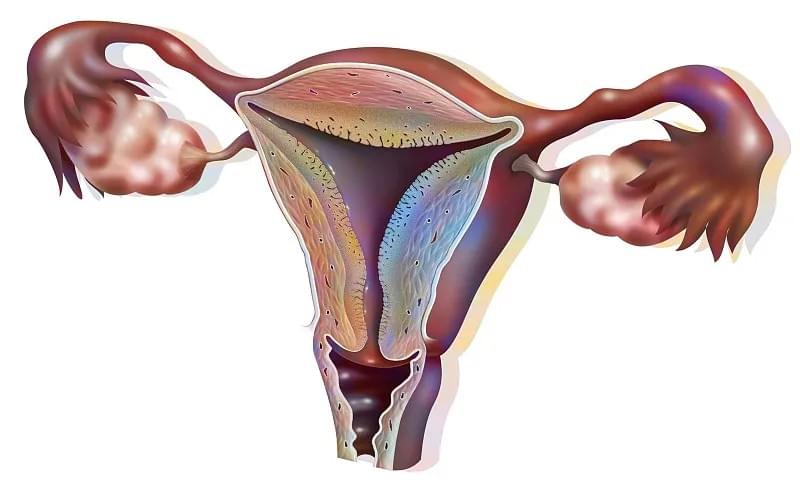
Ovulation is the process in which a mature egg is released from one of the ovaries into the fallopian tube, where it becomes available for fertilization. This typically occurs around day 14 of a 28-day menstrual cycle, although timing can vary from person to person.
Ovulation is a key part of the menstrual cycle and is essential for conception. Without ovulation, pregnancy cannot occur naturally. The process is regulated by a complex interplay of hormones, including:
- Follicle-Stimulating Hormone (FSH) – Stimulates follicle growth in the ovaries.
- Luteinizing Hormone (LH) – Triggers the release of the egg.
- Estrogen – Thickens the uterine lining and helps regulate the cycle.
- Progesterone – Prepares the uterus for implantation after ovulation.
When ovulation occurs, the corpus luteum (the remains of the follicle after egg release) produces progesterone, which stabilizes the endometrial lining. If fertilization doesn’t happen, progesterone levels drop, leading to menstruation.
But here’s where it gets interesting: you can still have bleeding that looks like a period—even if ovulation never happened.
Can You Have a Period Without Ovulating?
Yes, absolutely. What many people refer to as a “period” is actually any form of vaginal bleeding that occurs cyclically. However, true menstruation is defined as the shedding of the endometrial lining after the corpus luteum regresses due to lack of pregnancy—a process that only happens after ovulation.
In an anovulatory cycle, the body may still shed the uterine lining, but the hormonal triggers are different. This type of bleeding is often called anovulatory bleeding or dysfunctional uterine bleeding (DUB).
Here’s how it works:
- Estrogen Builds the Lining: Even without ovulation, the ovaries may still produce estrogen, which causes the endometrium (uterine lining) to thicken over time.
- No Progesterone Spike: Without ovulation, there’s no corpus luteum, so progesterone is not produced.
- Unstable Lining Breaks Down: The thickened lining, unsupported by progesterone, eventually becomes too heavy and unstable. It breaks down and sheds, resulting in bleeding that mimics a period.
This explains why someone can have seemingly regular cycles but still struggle with infertility or receive a diagnosis of anovulation.
How Common Are Anovulatory Cycles?
Anovulatory cycles are surprisingly common, especially during certain life stages:
- Adolescents: Up to 50% of cycles in the first year after menarche (first period) may be anovulatory.
- Perimenopausal Women: As ovarian reserve declines, anovulation becomes more frequent.
- Women with PCOS: Polycystic Ovary Syndrome is one of the leading causes of chronic anovulation.
- Athletes or Those with Low Body Weight: Intense physical activity or low body fat can suppress ovulation.
Even women with regular 28-day cycles may experience occasional anovulatory cycles due to stress, illness, or lifestyle changes.
Signs You Might Not Be Ovulating
While some anovulatory cycles go unnoticed, there are subtle clues that may indicate ovulation isn’t occurring:
- Irregular Cycle Length: Cycles shorter than 21 days or longer than 35 days.
- Bleeding That’s Heavier or Lighter Than Usual: Anovulatory bleeding can vary significantly in flow.
- Absence of Typical Ovulation Symptoms: No mid-cycle pain (mittelschmerz), no change in cervical mucus, or no rise in basal body temperature.
- Difficulty Conceiving: Infertility is often the first sign of chronic anovulation.
- Hormonal Acne or Excess Hair Growth: May indicate conditions like PCOS.
However, many women with anovulatory cycles have no symptoms at all, making it a silent issue until investigated.

What Causes Anovulation?
Anovulation is not a diagnosis in itself—it’s a symptom of an underlying hormonal or physiological imbalance. Here are the most common causes:
1. Polycystic Ovary Syndrome (PCOS)
PCOS affects up to 10% of women of reproductive age and is the most common cause of chronic anovulation. In PCOS, high levels of androgens (male hormones) and insulin resistance disrupt the normal ovulation process. Women with PCOS often have irregular periods, cysts on the ovaries, and symptoms like acne or hirsutism.
2. Hypothalamic Dysfunction
The hypothalamus in the brain controls the release of FSH and LH. Stress, extreme weight loss, excessive exercise, or eating disorders can suppress this system, leading to hypothalamic amenorrhea—a condition where ovulation stops, though some may still experience light bleeding.
3. Premature Ovarian Insufficiency (POI)
Also known as premature menopause, POI occurs when the ovaries stop functioning before age 40. Women may still have periods, but ovulation is infrequent or absent.
4. Thyroid Disorders
Both hypothyroidism and hyperthyroidism can interfere with the menstrual cycle and ovulation. The thyroid gland plays a key role in regulating metabolism and hormone production.
5. Hyperprolactinemia
High levels of prolactin—a hormone that stimulates milk production—can suppress ovulation. This can be caused by pituitary tumors, certain medications, or chronic stress.
6. Obesity or Low Body Weight
Excess body fat can increase estrogen production (since fat tissue converts androgens to estrogen), disrupting the hormonal balance. Conversely, very low body weight can shut down reproductive function as a survival mechanism.
7. Perimenopause
As women approach menopause, ovulation becomes less predictable. Anovulatory cycles are common during this transition, even if periods appear regular.
How Is Anovulation Diagnosed?
If you suspect you’re not ovulating, it’s important to consult a healthcare provider. Diagnosis typically involves a combination of:
- Medical History and Symptom Review: Including cycle patterns, weight changes, stress levels, and medication use.
- Blood Tests: To check hormone levels such as FSH, LH, estrogen, progesterone, thyroid hormones, and prolactin. A mid-luteal progesterone test (taken 7 days before expected period) can confirm whether ovulation occurred.
- Pelvic Ultrasound: To examine the ovaries for signs of PCOS or other structural issues.
- Ovulation Predictor Kits (OPKs): While not diagnostic, consistently negative OPKs over several cycles may suggest anovulation.
It’s important to note that tracking basal body temperature (BBT) can also help identify anovulatory cycles. In a normal cycle, BBT rises after ovulation due to progesterone. In an anovulatory cycle, no sustained temperature rise occurs.
Can You Get Pregnant Without Ovulating?
No. Pregnancy requires a mature egg to be released and fertilized by sperm. Without ovulation, conception cannot occur naturally.
However, many women with anovulation can still become pregnant with appropriate treatment. The key is identifying and addressing the underlying cause.
Treatment Options for Anovulation
Treatment depends on the cause, your age, and whether you’re trying to conceive. Here are common approaches:
1. Lifestyle Modifications
For many women, especially those with PCOS or weight-related anovulation, lifestyle changes can restore ovulation:
- Weight Management: Losing 5–10% of body weight can significantly improve ovulation in overweight women.
- Balanced Diet: Focus on whole grains, lean proteins, healthy fats, and low-glycemic foods to support insulin sensitivity.
- Regular Exercise: Moderate activity helps regulate hormones and reduce stress.
- Stress Reduction: Practices like yoga, meditation, or cognitive behavioral therapy can help rebalance the hypothalamic-pituitary-ovarian axis.
2. Medications to Induce Ovulation
- Clomiphene Citrate (Clomid): A first-line treatment that stimulates the pituitary gland to release more FSH and LH.
- Letrozole (Femara): Originally a breast cancer drug, it’s now widely used for ovulation induction, especially in women with PCOS.
- Metformin: Helps improve insulin sensitivity in women with PCOS, which can restore ovulation.
- Gonadotropins: Injectable hormones used when oral medications fail.
3. Treating Underlying Conditions
- Thyroid medication for hypothyroidism.
- Dopamine agonists for hyperprolactinemia.
- Hormonal birth control to regulate cycles (though this suppresses ovulation, it’s used for symptom management, not fertility).
4. Assisted Reproductive Technologies (ART)
For those struggling with infertility due to chronic anovulation, options like intrauterine insemination (IUI) or in vitro fertilization (IVF) may be recommended.

Myths and Misconceptions About Anovulation
Let’s clear up some common misunderstandings:
- Myth: “If I have regular periods, I must be ovulating.”
Truth: Regular bleeding does not guarantee ovulation. Anovulatory cycles can be predictable in timing.
- Myth: “Only women with PCOS have anovulation.”
Truth: Many conditions and factors can cause anovulation, including stress, thyroid issues, and aging.
- Myth: “Anovulation means I can’t get pregnant at all.”
Truth: While ovulation is necessary for conception, many women with anovulation can and do become pregnant with treatment.
- Myth: “Birth control pills fix anovulation.”
Truth: Birth control suppresses ovulation; it doesn’t restore it. It manages symptoms but doesn’t treat the root cause.
When to See a Doctor
You should consult a healthcare provider if:
- You’ve been trying to conceive for 12 months (or 6 months if over 35) without success.
- Your periods are irregular, very heavy, or absent.
- You have symptoms of hormonal imbalance (acne, hair loss, excess facial hair).
- You experience sudden changes in your cycle.
Early diagnosis and treatment can prevent long-term complications like infertility, endometrial hyperplasia, or even uterine cancer (due to unopposed estrogen).
Supporting Your Reproductive Health Naturally
While medical treatment is often necessary, daily habits can support hormonal balance:
- Track Your Cycle: Use apps or paper charts to monitor cycle length, symptoms, and bleeding patterns.
- Prioritize Sleep: Poor sleep disrupts cortisol and reproductive hormones.
- Limit Alcohol and Caffeine: Both can affect hormone metabolism.
- Consider Supplements: Inositol (for PCOS), vitamin D, omega-3 fatty acids, and magnesium may support ovulation—always consult your doctor first.

Final Thoughts
Experiencing periods without ovulating is more common than many realize—and it’s not something to ignore, especially if you’re planning for pregnancy or concerned about your long-term health. Anovulatory cycles are a sign that your body’s hormonal system is out of balance, and while they may not always cause obvious symptoms, they can have significant implications.
The good news? In most cases, anovulation is treatable. Whether through lifestyle changes, medication, or medical intervention, many women go on to restore regular ovulation and achieve their reproductive goals.
If you’re wondering whether you’re ovulating, don’t rely solely on the presence of a period. Talk to your doctor, consider tracking your cycle more closely, and take proactive steps to understand your body.
Your menstrual cycle is a vital sign of your overall health—not just a fertility indicator. Listening to it can lead to better outcomes, both for conception and long-term wellness.
