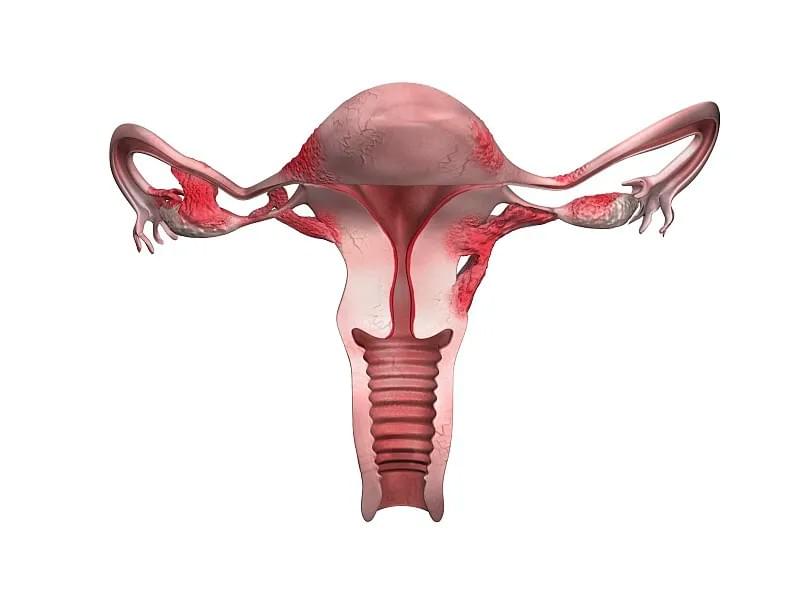
Endometriosis is a chronic and often painful condition affecting an estimated 1 in 10 women of reproductive age worldwide. Characterized by the growth of endometrial-like tissue outside the uterus—commonly on the ovaries, fallopian tubes, bowel, and pelvic lining—this disorder can lead to inflammation, scarring, and fertility challenges. For many women, a diagnosis of endometriosis brings not only physical discomfort but also emotional stress, especially when considering pregnancy. A common and deeply personal question arises: Can I get pregnant with endometriosis? The answer, while complex, is generally hopeful: yes, many women with endometriosis can and do have successful pregnancies, though the journey may require careful planning, medical support, and patience.
This comprehensive guide explores what it means to be pregnant with endometriosis, from conception challenges and symptom changes during pregnancy to potential complications and postpartum considerations. Whether you’ve recently been diagnosed, are trying to conceive, or are already expecting, this article provides evidence-based insights to help you navigate your unique path.
Understanding Endometriosis and Fertility
To fully appreciate the relationship between endometriosis and pregnancy, it’s essential to understand how the condition affects fertility. Endometriosis can interfere with conception in several ways:
- Anatomical Distortion: Scar tissue (adhesions) and ovarian cysts (endometriomas) can distort pelvic anatomy, obstructing the fallopian tubes or impairing egg release.
- Inflammation: Chronic pelvic inflammation may create a hostile environment for sperm, eggs, or embryos.
- Hormonal Imbalances: Altered hormone signaling can disrupt ovulation and implantation.
- Immune System Dysfunction: Some research suggests immune factors may play a role in rejecting embryos.
Despite these challenges, studies show that approximately 30% to 50% of women with endometriosis experience infertility, meaning a significant number do conceive naturally. Moreover, advances in assisted reproductive technologies (ART), such as in vitro fertilization (IVF), have greatly improved pregnancy outcomes for those who face difficulties.
Can Pregnancy Happen Naturally with Endometriosis?
Many women wonder if they must rely on fertility treatments to conceive. While severe endometriosis may necessitate intervention, mild to moderate cases often allow for natural conception. Research indicates that early-stage endometriosis (Stage I-II) has less impact on fertility than advanced stages (III-IV).
Timing is crucial. Experts recommend trying to conceive sooner rather than later after diagnosis, especially if surgery has been performed to remove endometrial lesions. Studies suggest a "window of opportunity" in the first 6 to 12 months post-surgery when fertility rates are temporarily improved due to reduced inflammation and restored anatomy.
However, it's important not to rush into pregnancy without proper preparation. Preconception counseling with a reproductive endocrinologist can help assess ovarian reserve, tubal patency, and overall reproductive health. Lifestyle factors—such as maintaining a healthy weight, reducing alcohol intake, quitting smoking, and managing stress—can also enhance fertility potential.
For couples struggling to conceive, options like intrauterine insemination (IUI) or IVF offer viable pathways. IVF, in particular, bypasses many of the mechanical barriers caused by endometriosis and has high success rates even in advanced cases.
How Pregnancy Affects Endometriosis Symptoms
One of the most frequently asked questions by expectant mothers with endometriosis is: Will pregnancy make my symptoms better or worse? The answer varies, but many women report significant symptom relief during pregnancy.
The hormonal shifts of pregnancy—particularly high levels of progesterone and the absence of menstruation—can suppress endometrial lesion activity. Progesterone has an anti-inflammatory effect and inhibits the growth of endometrial tissue. As a result, pelvic pain, dysmenorrhea (painful periods), and dyspareunia (pain during intercourse) often diminish or disappear entirely during gestation.
However, this relief is not universal. Some women continue to experience pain, especially if endometriosis involves deep infiltrating lesions or extra-pelvic sites (e.g., bowel or bladder). In rare cases, pregnancy may exacerbate symptoms due to increased blood flow and organ displacement in the pelvis.
It's also worth noting that while pregnancy may provide temporary remission, it is not a cure. Symptoms typically return after childbirth, particularly once menstrual cycles resume.

Potential Pregnancy Complications Linked to Endometriosis
While many pregnancies in women with endometriosis proceed normally, research indicates a slightly increased risk of certain complications. Awareness and early monitoring can help mitigate these risks.
1. Miscarriage
Some studies suggest a higher miscarriage rate among women with endometriosis, particularly those with advanced disease. This may be linked to impaired implantation or altered immune responses. However, data remains inconsistent, and many women go on to have healthy pregnancies.
2. Ectopic Pregnancy
Due to possible tubal damage or adhesions, the risk of ectopic (tubal) pregnancy may be elevated. Early ultrasound monitoring is recommended for women with a history of pelvic surgery or known tubal involvement.
3. Placenta Previa
Several large cohort studies have found a two- to threefold increased risk of placenta previa—a condition where the placenta covers the cervix—in women with endometriosis. This may be due to abnormal uterine receptivity or inflammation affecting implantation site selection.
4. Cesarean Delivery
Women with endometriosis are more likely to deliver via cesarean section. This may be due to prior surgeries causing adhesions, concerns about pelvic anatomy, or obstetric complications like malpresentation.
5. Preterm Birth and Low Birth Weight
Emerging evidence suggests a modest increase in preterm delivery and low birth weight, possibly related to systemic inflammation. Close prenatal care and lifestyle management are key to reducing these risks.
Despite these potential issues, most complications are manageable with proper medical supervision. Regular ultrasounds, maternal-fetal medicine consultations, and open communication with healthcare providers are essential.
Managing Endometriosis During Pregnancy
There is no standardized treatment protocol for active endometriosis during pregnancy, as most medications used outside of pregnancy (like hormonal contraceptives or GnRH agonists) are contraindicated. Therefore, management focuses on symptom monitoring and supportive care.
Pain during pregnancy should never be dismissed. While some discomfort is normal, persistent or severe pelvic pain warrants evaluation to rule out complications such as bowel obstruction (in cases of deep infiltrating endometriosis) or ovarian cyst rupture.
Conservative measures—such as rest, warm compresses, prenatal yoga, and physical therapy—can help manage mild symptoms. Always consult your OB-GYN before starting any new regimen.
Surgical intervention during pregnancy is extremely rare and only considered in life-threatening situations, such as acute bowel obstruction or hemorrhagic cysts. Most experts advise against elective surgery during gestation due to fetal risks.

Postpartum Considerations and Long-Term Outlook
After delivery, the focus often shifts back to managing endometriosis. Breastfeeding may delay the return of menstruation and associated pain, offering temporary relief due to its natural suppression of ovulation. However, symptoms typically reappear within months of weaning.
Women who have had endometriosis-related fertility treatments or surgeries should discuss long-term management strategies with their gynecologist. Options include hormonal therapies (progestins, combined oral contraceptives, or IUDs) to prevent recurrence, or further surgical interventions if necessary.
Importantly, having one successful pregnancy does not guarantee future fertility. Endometriosis is a progressive condition, and new lesions can develop over time. Those wishing to expand their families may consider fertility preservation (egg or embryo freezing) earlier rather than later.
Moreover, mental health support is vital. The emotional toll of living with a chronic illness, navigating fertility challenges, and adapting to motherhood can be overwhelming. Support groups, counseling, and patient advocacy organizations offer valuable resources.

Conclusion: Empowerment Through Knowledge
Being pregnant with endometriosis presents unique challenges, but it is far from a barrier to motherhood. With advancements in reproductive medicine, improved diagnostic tools, and greater awareness, more women than ever are achieving their dreams of building a family.
The key lies in proactive care: seeking early diagnosis, working with knowledgeable specialists, and staying informed about your options. Every woman’s experience is different, and there is no “one-size-fits-all” approach. But by understanding the interplay between endometriosis and pregnancy, you can advocate for yourself, minimize risks, and embrace the journey with confidence.
If you’re planning a pregnancy or already expecting, don’t hesitate to ask questions, request second opinions, and build a care team you trust. Your health—and your baby’s—depends on it.
Remember: Endometriosis may shape your path, but it doesn’t define your destiny.
