Ovulation is one of the most critical phases in the female reproductive cycle, yet it remains a topic shrouded in mystery for many. Whether you're trying to conceive, avoid pregnancy, or simply understand your body better, knowing what happens during ovulation can provide invaluable insight into your overall health and fertility. In this in-depth guide, we’ll explore the science behind ovulation, its hormonal triggers, physical signs, timing, and common misconceptions—offering a clear, evidence-based explanation that’s both informative and accessible.
Understanding the Menstrual Cycle: The Foundation of Ovulation
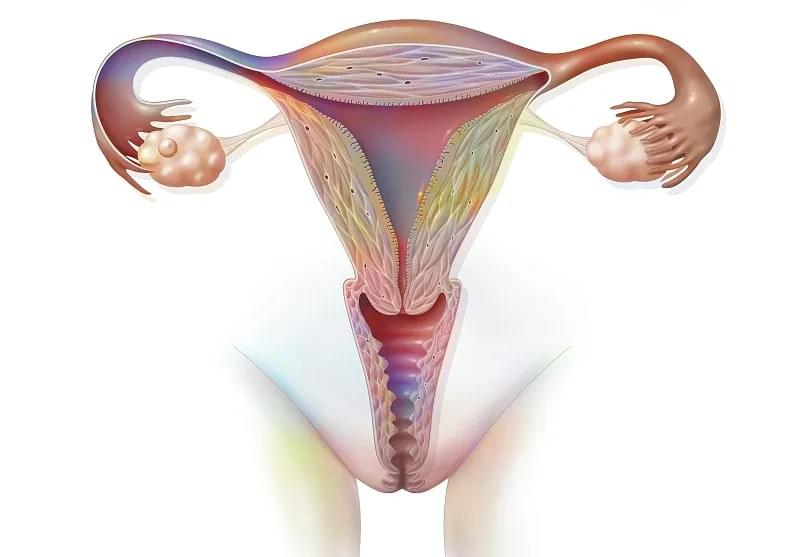
Before diving into the specifics of ovulation, it’s essential to understand the broader context: the menstrual cycle. The average menstrual cycle lasts about 28 days, though cycles ranging from 21 to 35 days are considered normal. This cycle is divided into four main phases:
- Menstruation (Days 1–5): The shedding of the uterine lining.
- Follicular Phase (Days 1–13): Development of ovarian follicles under the influence of follicle-stimulating hormone (FSH).
- Ovulation (Day 14, typically): The release of a mature egg from the ovary.
- Luteal Phase (Days 15–28): Preparation of the uterus for potential implantation; ends with menstruation if pregnancy does not occur.
Ovulation marks the transition from the follicular phase to the luteal phase and is the only time during the cycle when conception is possible.
The Hormonal Symphony Behind Ovulation
Ovulation is not a random event—it’s a precisely orchestrated process driven by a cascade of hormones. The hypothalamus, pituitary gland, and ovaries work in harmony to regulate this process.
1. Follicle-Stimulating Hormone (FSH) and Follicle Development
At the beginning of the cycle, the pituitary gland releases FSH, which stimulates several ovarian follicles to mature. Each follicle contains an immature egg (oocyte). Typically, only one follicle becomes dominant, while the others regress.
2. Estrogen Surge and the LH Surge
As the dominant follicle grows, it produces increasing amounts of estrogen. When estrogen levels reach a critical threshold—usually around day 12–13—this signals the hypothalamus to release gonadotropin-releasing hormone (GnRH), which in turn prompts the pituitary gland to release a surge of luteinizing hormone (LH).
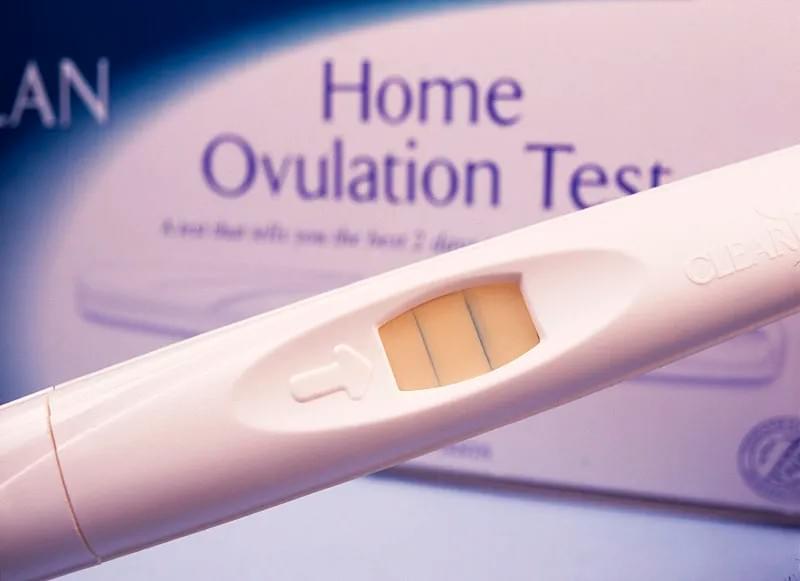
This LH surge is the key trigger for ovulation. It occurs approximately 24–36 hours before the egg is released and is the primary marker used in ovulation predictor kits (OPKs).
3. The Moment of Ovulation
About 36 hours after the LH surge begins, the mature follicle ruptures, releasing the egg into the fallopian tube. This is ovulation. The egg is then swept up by the fimbriae—finger-like projections at the end of the fallopian tube—and begins its journey toward the uterus.
The released egg remains viable for fertilization for only 12 to 24 hours, making timing crucial for conception.
Physical and Biological Changes During Ovulation
While ovulation is primarily a hormonal and internal process, it often comes with noticeable physical and physiological changes. These signs can help women identify their fertile window.
Cervical Mucus Changes
One of the most reliable natural indicators of fertility is cervical mucus. As estrogen rises before ovulation, the mucus becomes clear, stretchy, and slippery—resembling raw egg whites. This fertile-quality mucus helps sperm survive and travel through the cervix.
After ovulation, progesterone causes the mucus to become thicker and less hospitable to sperm.
Basal Body Temperature (BBT) Shift
A woman’s basal body temperature (BBT)—her temperature at rest—drops slightly just before ovulation and then rises by about 0.5°F (0.3°C) after ovulation due to increased progesterone. This biphasic pattern, when tracked daily, can confirm that ovulation has occurred.
However, BBT only indicates ovulation after it has happened, making it less useful for predicting the fertile window in real time.
Mittelschmerz: Ovulation Pain
Some women experience mittelschmerz, a German term meaning "middle pain," referring to mild cramping or twinges on one side of the lower abdomen around the time of ovulation. This pain can last from a few minutes to several hours and is caused by the follicle rupturing or irritation from follicular fluid.
Increased Libido and Other Subtle Signs
Research suggests that women may experience a natural increase in libido during their fertile window, likely an evolutionary mechanism to enhance the chances of conception. Other possible signs include breast tenderness, light spotting, bloating, and heightened senses of smell or vision.
Timing Ovulation: When Does It Really Happen?
Contrary to popular belief, ovulation does not always occur on day 14 of the menstrual cycle. While this may be average, the timing varies significantly from woman to woman—and even from cycle to cycle in the same individual.
- In a 28-day cycle, ovulation typically occurs around day 14.
- In a 35-day cycle, it may occur around day 21.
- In shorter cycles (e.g., 21 days), ovulation may happen as early as day 7.
Ovulation generally occurs about 14 days before the next period starts, regardless of cycle length. Therefore, women with irregular cycles may find it more challenging to predict ovulation without tracking methods.

How Long Is the Fertile Window?
While the egg only survives for up to 24 hours, the fertile window extends beyond ovulation day due to sperm longevity.
Sperm can survive in the female reproductive tract for up to 5 days under optimal conditions (i.e., in the presence of fertile cervical mucus). Therefore, the fertile window includes:
- The 5 days leading up to ovulation
- The day of ovulation itself
This means that intercourse as early as 5 days before ovulation can result in pregnancy. The two days before ovulation and the day of ovulation are the most fertile.
Understanding this window is crucial for both conception and natural family planning.
Methods to Track Ovulation Accurately
For women trying to conceive or avoid pregnancy, accurately identifying ovulation is essential. Here are several reliable methods:
1. Ovulation Predictor Kits (OPKs)
These urine-based tests detect the LH surge, indicating that ovulation will occur within the next 24–36 hours. They are over 90% accurate when used correctly but can be less reliable in women with polycystic ovary syndrome (PCOS) or irregular cycles.
2. Fertility Monitors
Advanced devices that track multiple hormones (LH and estrogen) in urine or saliva. Some even sync with smartphone apps to provide personalized predictions.
3. Basal Body Temperature (BBT) Charting
While not predictive, consistent BBT tracking helps confirm ovulation and identify patterns over time. Digital thermometers and fertility apps make this process easier.
4. Cervical Position and Mucus Monitoring
Women can learn to observe changes in cervical mucus and even check cervical position (which becomes higher, softer, and more open during fertility).
5. Transvaginal Ultrasound
Used in clinical settings, ultrasounds can monitor follicle growth and precisely time ovulation. This is often used during fertility treatments like IUI or IVF.
Common Misconceptions About Ovulation
Despite growing awareness, several myths persist about ovulation:
Myth 1: You Can’t Get Pregnant During Your Period
While unlikely, it’s not impossible. Women with short cycles or long periods may ovulate shortly after menstruation ends. Sperm can survive for days, so intercourse near the end of a period could lead to pregnancy.
Myth 2: All Women Ovulate on Day 14
As explained, ovulation timing varies widely. Relying on a "day 14" rule can lead to inaccurate fertility predictions.
Myth 3: Irregular Periods Mean You’re Not Ovulating
Some women with irregular cycles do ovulate, just unpredictably. Others may experience anovulatory cycles (no ovulation), which can be caused by stress, hormonal imbalances, or conditions like PCOS.
Myth 4: Ovulation Always Causes Obvious Symptoms
Many women experience no noticeable signs of ovulation. Lack of symptoms doesn’t mean ovulation isn’t occurring.
When Ovulation Doesn’t Happen: Anovulation
Anovulation—the absence of ovulation—is a common cause of infertility. It can result from:
- Polycystic Ovary Syndrome (PCOS)
- Thyroid disorders
- Excessive stress or exercise
- Low body weight or eating disorders
- Perimenopause
Women who consistently miss periods or have cycles longer than 35 days should consult a healthcare provider to evaluate ovulatory function.
Diagnosis may involve blood tests (progesterone, LH, FSH, thyroid hormones) and ultrasound imaging.
Supporting Healthy Ovulation: Lifestyle and Nutrition
While ovulation is a natural biological process, certain lifestyle factors can support or disrupt it.
1. Balanced Nutrition
A diet rich in whole grains, healthy fats (like omega-3s), lean proteins, and antioxidants supports hormonal balance. Studies suggest that foods like full-fat dairy, leafy greens, and complex carbohydrates may positively influence fertility.
2. Maintain a Healthy Weight
Both underweight and overweight conditions can disrupt hormonal balance and lead to irregular or absent ovulation.
3. Manage Stress
Chronic stress elevates cortisol, which can interfere with GnRH and disrupt the entire ovulatory process. Mindfulness, yoga, and adequate sleep can help regulate stress hormones.
4. Limit Alcohol and Caffeine
Excessive alcohol and caffeine intake may negatively impact fertility. Moderation is key.
5. Avoid Smoking
Smoking is linked to reduced ovarian reserve and earlier menopause.

Ovulation and Fertility Treatments
For couples struggling with infertility, understanding ovulation is the first step in diagnosis and treatment.
- Clomiphene Citrate (Clomid) and Letrozole are medications that stimulate ovulation by promoting FSH release.
- Gonadotropins are injectable hormones used in more advanced fertility treatments.
- Intrauterine Insemination (IUI) and In Vitro Fertilization (IVF) rely on precise ovulation timing or controlled ovarian stimulation.
Even in assisted reproduction, the principles of ovulation remain central.
Conclusion: Empowerment Through Knowledge
Ovulation is far more than just the release of an egg—it’s a complex, dynamic process that reflects the intricate balance of the female endocrine system. By understanding what happens during ovulation, women gain powerful insights into their fertility, health, and bodily autonomy.
Whether you’re planning a pregnancy, practicing natural contraception, or simply seeking to deepen your self-knowledge, tracking and understanding ovulation can be a transformative experience. With the right tools and awareness, you can navigate your cycle with confidence and clarity.
For healthcare providers, educators, and website operators aiming to support women’s health, providing accurate, accessible information about ovulation is not just informative—it’s empowering.
By demystifying this natural process, we help women take control of their reproductive health, one cycle at a time.
