Are you wondering if you can get pregnant? Discover 10 common signs that may indicate fertility issues, what they mean, and the next steps to take. Learn when to consult a specialist and how to improve your chances of conception.
Trying to conceive can be an emotional journey, especially when it doesn’t happen as quickly as expected. While occasional delays are normal, certain signs may indicate underlying fertility challenges. If you’ve been actively trying to conceive for over a year (or six months if you’re over 35), or if you’re experiencing specific symptoms, it might be time to explore potential fertility concerns.
This article outlines 10 clear signs that you might be facing difficulties getting pregnant. Understanding these indicators can help you seek timely medical advice, reduce anxiety, and take proactive steps toward building your family.
1. Irregular or Absent Menstrual Cycles
One of the most telling signs of potential fertility issues is an irregular or absent menstrual cycle. A regular cycle—typically lasting between 21 and 35 days—indicates that ovulation is occurring consistently. If your periods are unpredictable, excessively long (over 35 days), or absent (a condition known as amenorrhea), it may suggest that you’re not ovulating regularly.
Why It Matters:
Ovulation is essential for conception. Without a mature egg being released each month, pregnancy cannot occur naturally. Conditions like Polycystic Ovary Syndrome (PCOS), thyroid disorders, or extreme stress can disrupt your cycle and interfere with ovulation.
What to Do:
Track your cycles for at least three months using a period-tracking app or calendar. If irregularities persist, consult a healthcare provider. Blood tests and ultrasounds can help diagnose hormonal imbalances or structural issues.

2. Extremely Painful Periods (Dysmenorrhea)
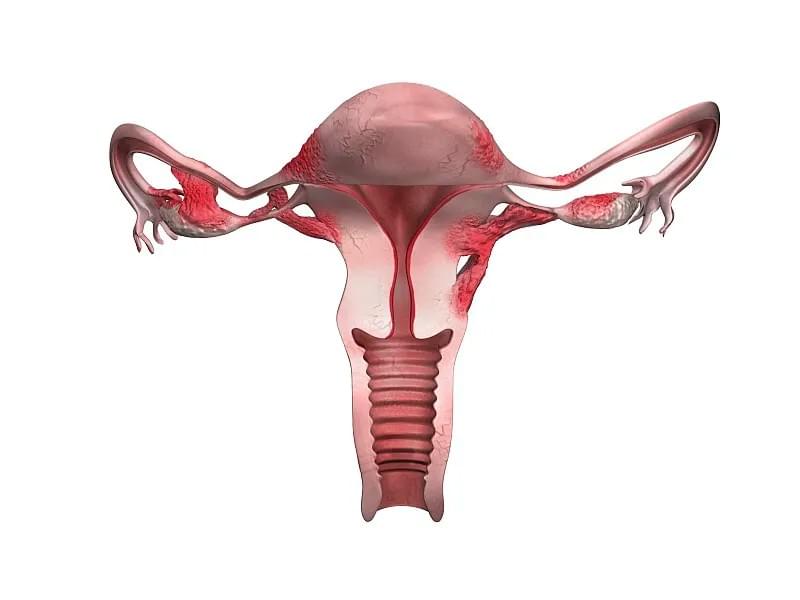
While mild cramping during menstruation is common, severe pain that interferes with daily life could be a red flag. Painful periods, especially when they worsen over time, may indicate endometriosis—a condition where tissue similar to the uterine lining grows outside the uterus.
Why It Matters:
Endometriosis affects up to 50% of women with infertility. The misplaced tissue can cause inflammation, scarring, and blockages in the fallopian tubes, making it difficult for sperm to reach the egg or for a fertilized egg to implant properly.
Symptoms to Watch For:
- Severe pelvic pain before and during periods
- Pain during or after sex
- Heavy menstrual bleeding
- Painful bowel movements or urination during menstruation
What to Do:
Don’t dismiss severe pain as “normal.” Speak to a gynecologist, especially if over-the-counter pain relievers aren’t effective. A laparoscopy may be needed for a definitive diagnosis.
3. History of Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease is an infection of the female reproductive organs, often caused by untreated sexually transmitted infections (STIs) like chlamydia or gonorrhea. Even if symptoms were mild or went unnoticed, PID can cause lasting damage.
Why It Matters:
PID can lead to scarring and blockages in the fallopian tubes, preventing the egg and sperm from meeting. It’s a leading cause of tubal factor infertility, which accounts for about 20-25% of infertility cases in women.
Silent Damage:
Many women don’t realize they’ve had PID because symptoms can be subtle—mild pelvic pain, unusual discharge, or no symptoms at all. By the time fertility issues arise, the damage may already be done.
What to Do:
If you’ve ever been diagnosed with an STI or suspect you might have had one, inform your doctor. A hysterosalpingogram (HSG)—an X-ray test that checks for blockages—can assess tube patency.

4. Recurrent Miscarriages
Experiencing one miscarriage is unfortunately common—about 10-20% of known pregnancies end this way. However, two or more consecutive miscarriages (recurrent pregnancy loss) may point to an underlying fertility issue.
Possible Causes:
- Chromosomal abnormalities in the embryo
- Uterine structural problems (e.g., fibroids, septate uterus)
- Autoimmune disorders (e.g., antiphospholipid syndrome)
- Hormonal imbalances (e.g., low progesterone)
Emotional Impact:
Recurrent miscarriages can be emotionally devastating. It’s important to remember that many causes are treatable, and with proper care, many women go on to have successful pregnancies.
What to Do:
After two miscarriages, consider a fertility evaluation. Tests may include genetic screening, hormone panels, and imaging of the uterus.
5. Age-Related Fertility Decline
While not a “symptom” per se, age is one of the most significant factors affecting fertility. Women are born with all the eggs they’ll ever have, and both egg quantity and quality decline with age.
Key Milestones:
- Fertility begins to decline gradually after age 32
- A more rapid decline occurs after age 37
- By age 40, the chance of conceiving naturally each month drops to about 5%
Why It Matters:
Older eggs are more likely to have chromosomal abnormalities, increasing the risk of miscarriage and conditions like Down syndrome. Men also experience age-related fertility decline, though more gradually.
What to Do:
If you’re over 35 and haven’t conceived after six months of trying, seek help. Options like egg freezing, IVF, or donor eggs may be discussed based on your situation.
6. Unexplained Weight Changes
Sudden or unexplained weight gain or loss can disrupt hormonal balance and affect fertility. Both extremes—being significantly underweight or overweight—can interfere with ovulation.
Underweight and Fertility:
Low body fat can stop ovulation entirely. This is common in athletes or those with eating disorders, as the body may not have enough energy reserves to support a pregnancy.
Overweight and Fertility:
Excess fat tissue can increase estrogen production, which disrupts the hormonal signals needed for ovulation. Obesity is also linked to insulin resistance, a factor in PCOS.
What to Do:
Aim for a healthy BMI (18.5–24.9). Even a 5–10% weight loss can restore ovulation in women with obesity-related infertility.
7. Male Partner’s Fertility Concerns
Infertility isn’t just a female issue—about one-third of cases are due to male factors. If your partner has a history of testicular injury, surgery (like hernia repair), low sperm count, or erectile dysfunction, it could affect your ability to conceive.
Common Male Fertility Issues:
- Low sperm count (oligospermia)
- Poor sperm motility (asthenospermia)
- Abnormal sperm morphology (teratospermia)
- Varicocele (enlarged veins in the scrotum)
What to Do:
A semen analysis is a simple, non-invasive test that can reveal male fertility issues. Early testing allows for timely interventions like lifestyle changes, medication, or assisted reproductive technologies.
8. History of Cancer Treatment
Cancer treatments like chemotherapy and radiation can have a lasting impact on fertility. These therapies target rapidly dividing cells, which includes both cancer cells and reproductive cells.
Risk Factors:
- Type and dosage of chemotherapy
- Radiation exposure to the pelvic area
- Age at the time of treatment
What to Do:
If you’ve undergone cancer treatment and are planning a family, consult a fertility specialist. Options like egg or sperm freezing before treatment, or using donor gametes afterward, may be available.
9. Chronic Health Conditions
Certain long-term health issues can interfere with fertility. These include:
- Diabetes: Poorly controlled blood sugar can affect ovulation and increase miscarriage risk.
- Autoimmune Diseases: Conditions like lupus or rheumatoid arthritis may impact implantation or increase inflammation.
- Thyroid Disorders: Both hypothyroidism and hyperthyroidism can disrupt menstrual cycles and ovulation.
What to Do:
Work with your healthcare provider to manage your condition. Optimizing your health before conception improves fertility outcomes and supports a healthy pregnancy.
10. No Known Issues, But Still Not Pregnant
Sometimes, couples do everything “right”—regular cycles, healthy lifestyle, timed intercourse—yet still don’t conceive. This is known as unexplained infertility, affecting about 10–30% of couples.
What It Means:
Unexplained infertility doesn’t mean there’s no cause; it means current tests haven’t identified it. It could involve subtle issues with egg quality, sperm function, or embryo development.
What to Do:
Don’t lose hope. Many couples with unexplained infertility achieve pregnancy with treatments like ovulation induction, intrauterine insemination (IUI), or in vitro fertilization (IVF).

When Should You See a Fertility Specialist?
The American Society for Reproductive Medicine (ASRM) recommends the following timelines:
- Under 35: Seek help after 12 months of unprotected intercourse without conception.
- 35 or older: Consult a specialist after 6 months.
- Known risk factors: Don’t wait—seek evaluation earlier if you have any of the signs mentioned above.
A fertility evaluation typically includes:
- Hormone testing (FSH, AMH, thyroid, prolactin)
- Ultrasound to assess ovarian reserve and uterine health
- Semen analysis for male partners
- Imaging tests (HSG or sonohysterogram) to check the uterus and tubes
Final Thoughts: You’re Not Alone
Struggling to conceive can feel isolating, but millions of people face similar challenges. Recognizing the signs of potential fertility issues is the first step toward getting the help you need.
Remember, infertility is a medical condition—not a personal failing. With advances in reproductive medicine, many couples go on to build families through treatments like IVF, IUI, or even lifestyle adjustments.
If you’re concerned about your fertility, don’t wait. Early evaluation increases your chances of success. Talk to your doctor, consider a referral to a reproductive endocrinologist, and take comfort in knowing that support and solutions are available.
Call to Action:
If you’ve been trying to conceive without success, take the next step today. Schedule a consultation with a fertility specialist and start your journey toward parenthood with confidence.
