Chlamydia is one of the most common sexually transmitted infections (STIs) worldwide, particularly affecting individuals between the ages of 15 and 24. While often discussed in broad terms, it’s crucial to understand how chlamydia specifically impacts men—not only in terms of immediate symptoms but also long-term health consequences if left untreated. This article provides a detailed exploration of chlamydia side effects for men, including physical manifestations, potential complications, diagnosis methods, treatment options, and preventive strategies. Whether you're seeking personal knowledge or supporting someone else, this guide aims to deliver accurate, up-to-date, and actionable information.
What Is Chlamydia?
Chlamydia is caused by the bacterium Chlamydia trachomatis, which thrives in warm, moist environments such as the genital tract, rectum, throat, and eyes. It spreads primarily through unprotected vaginal, anal, or oral sex with an infected partner. One of the reasons chlamydia remains so widespread is that many people—especially men—do not experience noticeable symptoms immediately after infection, allowing them to unknowingly transmit the bacteria to others.
According to data from the World Health Organization (WHO), there are over 127 million new cases of chlamydia globally each year. In the United States alone, the Centers for Disease Control and Prevention (CDC) reported more than 1.6 million cases in 2022, marking a steady increase over the past decade. These rising numbers underscore the importance of awareness, regular testing, and early intervention.
While women often receive significant attention in discussions about chlamydia due to risks like pelvic inflammatory disease (PID) and infertility, men are equally vulnerable to serious health issues when the infection goes undetected or untreated.
Common Side Effects of Chlamydia in Men
Many men infected with chlamydia remain asymptomatic for weeks or even months. However, when symptoms do appear, they typically develop within 1 to 3 weeks after exposure. Recognizing these signs early can significantly reduce the risk of complications.
1. Urethral Discharge
One of the most frequently reported symptoms among men is an abnormal discharge from the penis. This discharge may be clear, cloudy, or slightly yellowish and is usually noticeable upon waking or after urination. Unlike normal pre-ejaculate fluid, chlamydial discharge tends to persist throughout the day and may have a mild odor.
2. Painful Urination (Dysuria)
Burning or stinging sensations during urination are common indicators of urethral inflammation caused by chlamydia. The discomfort can range from mild irritation to sharp pain and is often mistaken for a urinary tract infection (UTI). However, unlike UTIs—which are less common in younger men—chlamydia-related dysuria stems from a sexually acquired bacterial infection.
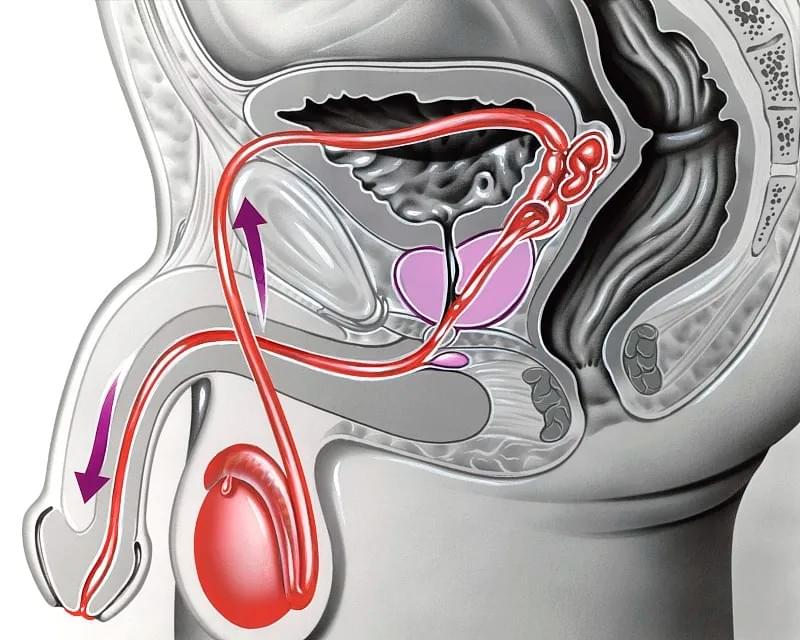
3. Testicular Pain or Swelling
In some cases, chlamydia can spread from the urethra to the epididymis—a tube located at the back of the testicle that stores and carries sperm. This condition, known as epididymitis, leads to pain, tenderness, and swelling in one or both testicles. If not treated promptly, epididymitis can impair fertility and lead to chronic discomfort.
4. Rectal Infection Symptoms
Men who engage in receptive anal intercourse may develop rectal chlamydia. Symptoms include rectal pain, discharge, bleeding, or a persistent feeling of needing to pass stool (tenesmus). Some describe a sensation of pressure or fullness in the lower abdomen. Because these symptoms mimic other gastrointestinal conditions like hemorrhoids or proctitis, rectal chlamydia is often underdiagnosed unless specific testing is performed.
5. Pharyngeal (Throat) Infections
Oral sex with an infected partner can result in pharyngeal chlamydia. Most cases are asymptomatic, but some men report a sore throat, mild hoarseness, or difficulty swallowing. Due to the lack of distinctive symptoms, throat infections are rarely self-identified and require targeted swab testing for detection.
Long-Term Complications: When Chlamydia Goes Untreated
The true danger of chlamydia lies in its ability to cause silent damage over time. Even in the absence of symptoms, the infection can progress and lead to severe complications.
Epididymo-Orchitis
When chlamydia ascends into the epididymis and testes, it can trigger epididymo-orchitis—a combination of epididymitis and orchitis (inflammation of the testicle). This condition causes intense pain, fever, and systemic illness. Chronic cases may result in scarring, reduced blood flow, and impaired sperm production, increasing the risk of male infertility.
Studies published in the Journal of Infectious Diseases suggest that untreated chlamydia contributes to approximately 10–15% of male factor infertility cases linked to genital tract infections. While fertility can sometimes recover after treatment, prolonged infection increases the likelihood of permanent damage.
Reactive Arthritis (Previously Known as Reiter’s Syndrome)
A small percentage of men—particularly those with the HLA-B27 genetic marker—may develop reactive arthritis following a chlamydia infection. This autoimmune response typically occurs 1–4 weeks after initial infection and presents with a triad of symptoms:
- Joint pain and swelling (often in the knees, ankles, or feet)
- Conjunctivitis (eye redness and irritation)
- Urethritis (inflammation of the urethra)
This condition can become chronic and debilitating, significantly impacting quality of life. Early antibiotic treatment may help mitigate severity, but managing reactive arthritis often requires ongoing rheumatological care.
Increased Risk of HIV Transmission
Chlamydia-induced inflammation creates micro-tears in mucosal tissues, making it easier for HIV and other STIs to enter the body during sexual contact. Research from the Lancet Infectious Diseases journal indicates that individuals with active chlamydia infections are up to three times more likely to acquire HIV if exposed. Furthermore, co-infected individuals may have higher viral loads, increasing their potential to transmit HIV to partners.
Prostatitis
Although less common, chlamydia can infect the prostate gland, leading to chronic bacterial prostatitis. Symptoms include pelvic pain, painful ejaculation, frequent urination, and lower back discomfort. Diagnosing chlamydial prostatitis requires specialized urine or semen cultures, as standard tests may miss the pathogen.
Diagnosis: How Is Chlamydia Detected in Men?
Early diagnosis is key to preventing complications. Fortunately, testing for chlamydia is simple, non-invasive, and highly accurate.
Nucleic Acid Amplification Tests (NAATs)
The gold standard for chlamydia detection is the NAAT, which analyzes DNA from a urine sample or swab. For men, a first-catch urine specimen (the initial part of the urine stream) provides excellent sensitivity and specificity. Rectal and throat swabs are recommended for men who have sex with men (MSM) or those reporting receptive anal/oral sex.
Testing should occur:
- At least once a year for sexually active men under 25
- More frequently for those with multiple or new sexual partners
- After any unprotected sexual encounter with a partner of unknown status
It's important to note that testing too soon after exposure (within 1–2 days) may yield false negatives, as the bacteria need time to multiply to detectable levels. Waiting at least 1–2 weeks post-exposure ensures reliable results.

Treatment Options and Recovery
Chlamydia is curable with appropriate antibiotics. The CDC currently recommends:
- Azithromycin 1 gram orally in a single dose, OR
- Doxycycline 100 mg twice daily for 7 days
Both regimens are highly effective, though doxycycline may offer slightly better eradication rates in certain populations. Alternative treatments (such as erythromycin or levofloxacin) are available for patients with allergies or contraindications.
Key Points During Treatment:
- Avoid all sexual activity for at least 7 days after starting antibiotics.
- Complete the full course of medication, even if symptoms disappear earlier.
- Inform all recent sexual partners (within the last 60 days) so they can get tested and treated.
- Get retested 3 months after treatment to ensure reinfection hasn’t occurred.
Partner notification is critical. Studies show that treating only the infected individual without addressing partners leads to reinfection rates as high as 20%. Digital tools like anonymous partner messaging services (e.g., Let Them Know, InSpot) can help facilitate communication while maintaining privacy.
Preventive Strategies: Reducing Your Risk
Prevention remains the best defense against chlamydia and its associated side effects.
1. Consistent Condom Use
Latex or polyurethane condoms significantly reduce the transmission of chlamydia during vaginal, anal, and oral sex. Proper usage—from start to finish—is essential; partial use diminishes protection.
2. Regular STI Screening
Annual screening is recommended for all sexually active men under 25, and for older men with risk factors (new/multiple partners, MSM, history of STIs). Routine check-ups normalize testing and catch infections before complications arise.
3. Mutual Monogamy and Open Communication
Being in a long-term, mutually monogamous relationship with a partner who has tested negative reduces risk. Honest conversations about sexual health, testing history, and boundaries foster trust and safety.
4. Vaccination and Future Prospects
Currently, no vaccine exists for chlamydia, but several candidates are in development. Researchers at the University of North Carolina and Imperial College London are conducting promising Phase I trials on subunit vaccines targeting major outer membrane proteins of C. trachomatis. While widespread availability is likely years away, vaccination could revolutionize prevention efforts in the future.

Myths vs. Facts About Chlamydia in Men
Misinformation fuels stigma and discourages testing. Let’s clarify some common misconceptions:
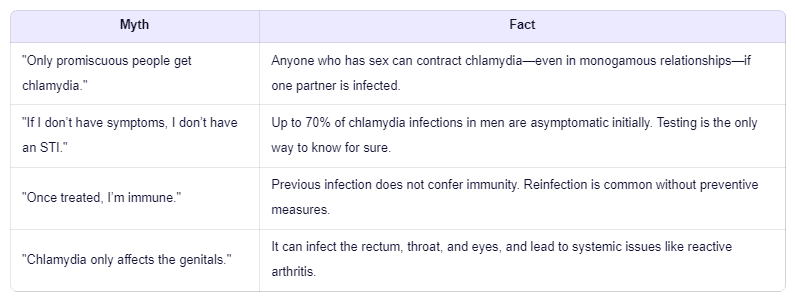
Dispelling these myths promotes healthier attitudes toward sexual wellness and encourages proactive healthcare behavior.
The Role of Telemedicine and At-Home Testing
Advancements in digital health have made chlamydia testing more accessible than ever. Many clinics now offer telehealth consultations where patients can discuss symptoms, order lab tests, and receive prescriptions online. At-home STI test kits allow discreet collection of urine or swab samples, which are mailed to certified labs for analysis.
These innovations remove barriers such as embarrassment, transportation challenges, or limited clinic hours. A 2023 study in Sexually Transmitted Infections found that men using at-home testing were 40% more likely to complete follow-up treatment compared to those relying on traditional clinic visits.
However, users must choose reputable providers accredited by organizations like CLIA (Clinical Laboratory Improvement Amendments) to ensure accuracy and confidentiality.

Conclusion: Take Charge of Your Sexual Health
Chlamydia may be common, but it is neither harmless nor inevitable. For men, understanding the potential side effects—from urethral discharge to infertility and reactive arthritis—is vital for early detection and prevention. With timely testing, effective treatment, and consistent protective measures, chlamydia can be managed successfully.
If you’re sexually active, make STI screening a routine part of your healthcare, just like annual physicals or dental check-ups. Encourage open dialogue with partners and healthcare providers. By normalizing conversations around sexual health, we can reduce stigma, improve outcomes, and build a safer, more informed community.
Remember: knowledge is power. Stay informed, stay protected, and prioritize your well-being.
