Ovulation is a fundamental biological process in the female reproductive system, playing a central role in fertility, hormonal balance, and overall women’s health. Despite its importance, many people—especially those not actively trying to conceive—remain unfamiliar with how ovulation works, when it occurs, and what signs to look for. This comprehensive guide aims to demystify ovulation, offering science-backed insights into its mechanisms, timing, symptoms, and implications for both conception and general wellness. Whether you're planning a pregnancy, tracking your cycle for health reasons, or simply seeking to understand your body better, this article provides essential knowledge that empowers informed decisions.
What Is Ovulation?
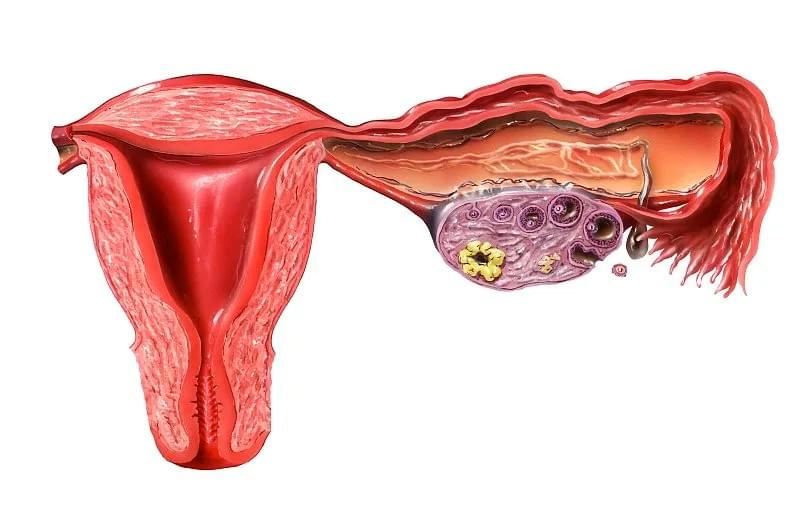
Ovulation is the process by which a mature egg (ovum) is released from one of the ovaries into the fallopian tube, where it becomes available for fertilization by sperm. This event is a pivotal moment in the menstrual cycle and typically occurs once per cycle in most women of reproductive age. While the average menstrual cycle lasts 28 days, ovulation does not always happen on day 14—a common misconception. In reality, the timing of ovulation can vary significantly from person to person and even from cycle to cycle within the same individual.
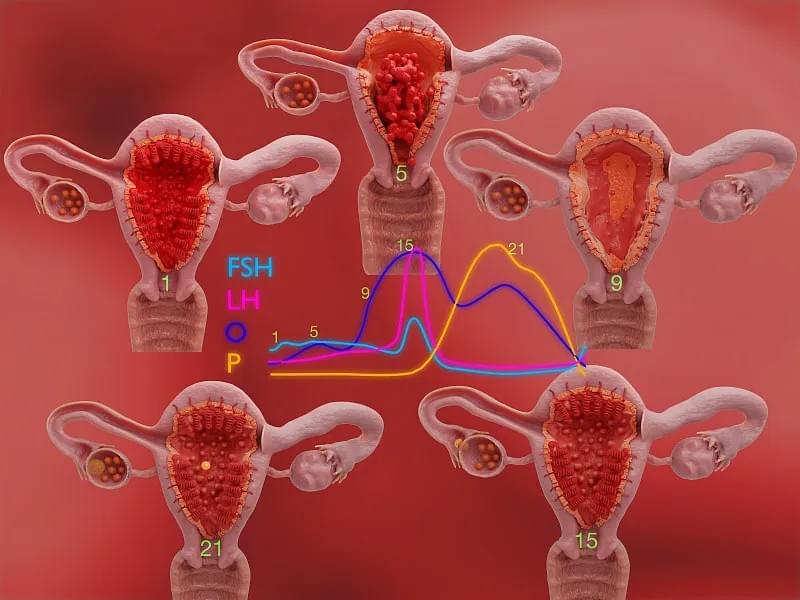
The process begins in the brain, where the hypothalamus signals the pituitary gland to release two key hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH stimulates the growth of several ovarian follicles, each containing an immature egg. Usually, only one follicle will fully mature and release its egg during ovulation, while the others degenerate. As the dominant follicle develops, it produces increasing amounts of estrogen, which eventually triggers a surge in LH. This LH surge is the immediate precursor to ovulation and usually occurs 24 to 36 hours before the egg is released.
Once released, the egg travels down the fallopian tube, where it can survive for up to 24 hours. If sperm are present during this window, fertilization may occur. If not, the egg disintegrates and is absorbed by the body or shed along with the uterine lining during menstruation.
When Does Ovulation Occur?
Pinpointing the exact day of ovulation requires more than just counting days from the start of your period. While a textbook 28-day cycle with ovulation on day 14 is often cited, research shows that only about 10% of women actually ovulate on day 14. A study published in Human Reproduction found that the majority of women ovulate earlier or later, with the most common range falling between day 12 and day 16.
Ovulation typically occurs about 14 days before the start of the next menstrual period, regardless of cycle length. For example:
- In a 26-day cycle, ovulation likely occurs around day 12.
- In a 32-day cycle, ovulation may occur around day 18.
This means that women with irregular cycles may find it more challenging to predict ovulation using calendar-based methods alone. Factors such as stress, illness, travel, and significant changes in weight or exercise routines can all influence the timing of ovulation, sometimes causing it to be delayed or skipped entirely.
It’s also important to note that ovulation can occur without menstruation (such as during breastfeeding or in certain hormonal disorders), and conversely, menstrual bleeding can occur without ovulation (known as anovulatory cycles). This distinction is crucial for women trying to conceive or avoid pregnancy, as relying solely on period tracking can be misleading.
Signs and Symptoms of Ovulation
The body often provides subtle—but detectable—clues that ovulation is approaching or has occurred. Recognizing these signs can help individuals better understand their fertility windows and reproductive health.
1. Changes in Cervical Mucus
One of the most reliable natural indicators of fertility is cervical mucus. As estrogen levels rise in the lead-up to ovulation, the mucus becomes clear, slippery, and stretchy—resembling raw egg whites. This consistency helps sperm travel through the cervix and into the uterus. After ovulation, progesterone causes the mucus to become thicker and less fertile.
2. Basal Body Temperature (BBT) Shift
A woman’s basal body temperature—the temperature upon waking—drops slightly just before ovulation and then rises by about 0.5 to 1.0 degree Fahrenheit after the egg is released. This temperature shift is caused by increased progesterone production and remains elevated until the next period begins. Tracking BBT daily with a specialized thermometer can help confirm that ovulation has occurred, though it cannot predict it in real time.
3. Mild Pelvic Pain (Mittelschmerz)
Some women experience a brief, one-sided lower abdominal pain during ovulation, known as mittelschmerz (German for "middle pain"). This sensation can last from a few minutes to a few hours and is thought to result from the follicle rupturing or irritation from fluid or blood released with the egg.
4. Increased Libido and Sensory Perception
Studies suggest that women may experience a natural increase in sexual desire around ovulation, possibly as an evolutionary mechanism to enhance reproductive success. Some also report heightened senses of smell, taste, or attractiveness during this phase.
5. Breast Tenderness and Bloating
Due to hormonal fluctuations, some women notice mild breast soreness or abdominal bloating mid-cycle. While these symptoms are more commonly associated with premenstrual syndrome (PMS), they can also appear during the ovulatory phase.

How to Track Ovulation Accurately
For those trying to conceive or avoid pregnancy naturally, accurate ovulation tracking is essential. While no single method is 100% foolproof, combining multiple approaches increases reliability.
1. Ovulation Predictor Kits (OPKs)
These urine-based tests detect the surge in luteinizing hormone (LH) that precedes ovulation. OPKs are widely available, easy to use, and highly accurate when used correctly. Testing is typically done in the afternoon or evening, as LH levels tend to rise during the day. A positive result usually indicates ovulation within the next 12 to 36 hours.
2. Fertility Monitors
Advanced devices analyze hormone levels in urine or saliva patterns to predict fertility. Some monitors track both estrogen and LH, providing a broader fertility window. Others use optical sensors to examine saliva for ferning patterns, which become more pronounced with rising estrogen.
3. Cycle Tracking Apps
Digital tools like Clue, Flo, or Natural Cycles allow users to log symptoms, temperatures, and test results. Over time, these apps can identify patterns and offer personalized predictions. However, they work best when combined with real-time data rather than relying solely on historical cycle averages.
4. Transvaginal Ultrasound
Used primarily in clinical settings, ultrasounds can monitor follicle development and confirm ovulation. This method is most common in fertility treatments like intrauterine insemination (IUI) or in vitro fertilization (IVF).
5. Blood Tests
Hormone panels can measure progesterone levels about one week after suspected ovulation. A progesterone level above 3 ng/mL is generally considered evidence of ovulation.
Common Myths About Ovulation
Despite growing awareness, several myths persist about ovulation, often leading to confusion or misinformation.
Myth 1: You Can’t Get Pregnant Right After Your Period
While the chances are lower, it’s possible—especially for women with short cycles or long periods. Sperm can survive up to five days in the reproductive tract, so if ovulation occurs shortly after menstruation ends, conception can occur.
Myth 2: Ovulation Always Happens on Day 14
As previously discussed, ovulation timing varies widely. Assuming it happens on day 14 can lead to mistimed intercourse or incorrect fertility assessments.
Myth 3: You Need to Have Sex Every Day to Conceive
While frequent intercourse during the fertile window increases odds, having sex every other day is often sufficient. Daily ejaculation can reduce sperm count, so balance is key.
Myth 4: Irregular Periods Mean You’re Not Ovulating
Some women with irregular cycles still ovulate, albeit unpredictably. Conversely, regular periods don’t guarantee ovulation—some cycles may be anovulatory.
Myth 5: Ovulation Pain Means You’re Definitely Ovulating
While mittelschmerz is associated with ovulation, not all women experience it, and some may feel similar pain due to other conditions like ovarian cysts or endometriosis.
Ovulation and Fertility: Maximizing Your Chances
For couples trying to conceive, understanding the fertile window is critical. This window includes the five days leading up to ovulation and the day of ovulation itself, as sperm can survive in the female reproductive tract for up to five days, while the egg survives only about 24 hours.
Experts recommend having intercourse every 1 to 2 days during this window to maximize the chances of conception. Research shows that the probability of pregnancy is highest when intercourse occurs in the two days before ovulation.
Lifestyle factors also play a significant role in fertility. Maintaining a healthy weight, avoiding smoking and excessive alcohol, managing stress, and eating a balanced diet rich in antioxidants, folic acid, and omega-3 fatty acids can support both male and female reproductive health.
For those experiencing difficulty conceiving, tracking ovulation can help identify potential issues, such as anovulation (lack of ovulation), which may be linked to conditions like polycystic ovary syndrome (PCOS), thyroid disorders, or premature ovarian insufficiency. In such cases, medical evaluation and treatment may be necessary.
Ovulation Beyond Conception: A Marker of Health
Ovulation is not just about fertility—it’s also a vital sign of hormonal and metabolic health. Regular ovulation indicates that the hypothalamic-pituitary-ovarian (HPO) axis is functioning properly and that key hormones are in balance.
When ovulation stops or becomes irregular, it can signal underlying health issues. For example:
- Polycystic Ovary Syndrome (PCOS): Characterized by irregular or absent ovulation, high androgen levels, and ovarian cysts.
- Hypothalamic Amenorrhea: Caused by extreme stress, low body weight, or excessive exercise, leading to suppressed ovulation.
- Thyroid Disorders: Both hyper- and hypothyroidism can disrupt ovulation.
- Perimenopause: As women approach menopause, ovulation becomes less frequent and more unpredictable.
Moreover, the hormone progesterone, produced after ovulation, has protective effects on the endometrium, reducing the risk of abnormal cell growth and endometrial cancer. Women who do not ovulate regularly may miss out on these benefits, increasing long-term health risks.
Therefore, tracking ovulation isn’t just for those trying to get pregnant—it’s a valuable tool for all women seeking to understand their bodies and maintain long-term wellness.

Conclusion: Embracing Ovulation Awareness
Ovulation is far more than a biological event tied to reproduction—it’s a window into a woman’s overall health and hormonal harmony. By learning to recognize the signs, track the timing, and understand the science behind ovulation, individuals gain greater control over their reproductive choices and long-term well-being.
Whether you're planning for a baby, avoiding pregnancy naturally, or simply aiming to tune into your body’s rhythms, ovulation awareness is a powerful form of self-knowledge. With the help of modern tools and a deeper understanding of individual variability, anyone can move beyond myths and embrace a more informed, empowered approach to reproductive health.
As healthcare continues to evolve toward personalized and preventive models, ovulation tracking stands out as a simple yet profound practice—one that bridges biology, technology, and personal agency. By sharing accurate, accessible information like this, we contribute to a world where women are not just informed about their bodies, but in command of them.
