Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders affecting women of reproductive age, with an estimated prevalence of 6% to 12% globally. Among its many challenges, infertility stands out as a primary concern for many women diagnosed with PCOS. While PCOS-related infertility can be distressing, modern medicine offers a range of effective treatment strategies that can significantly improve fertility outcomes. This comprehensive guide explores the latest evidence-based approaches to managing PCOS-related infertility, empowering women with knowledge and practical solutions to achieve their dream of motherhood.
Understanding the Link Between PCOS and Infertility
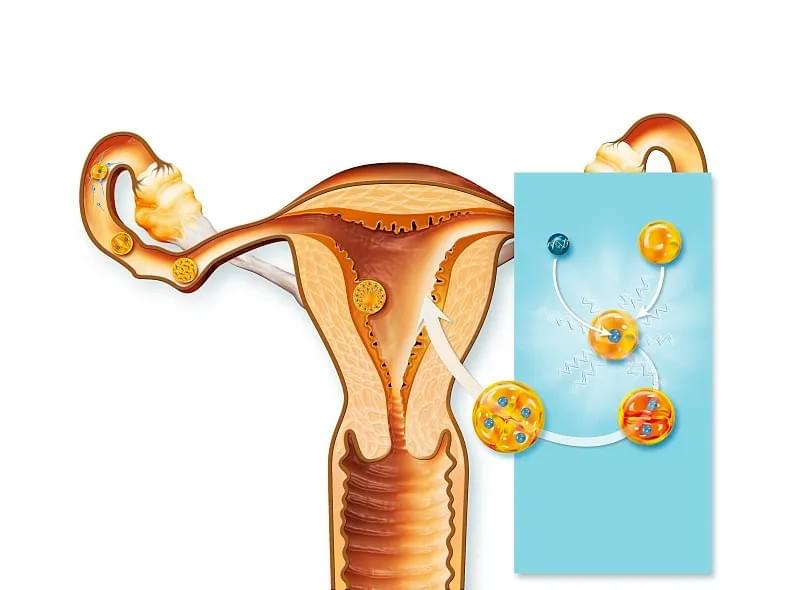
At its core, PCOS disrupts the normal hormonal balance required for regular ovulation. Women with PCOS often experience elevated levels of androgens (male hormones), insulin resistance, and irregular menstrual cycles—all of which contribute to anovulation, the primary cause of infertility in these cases.
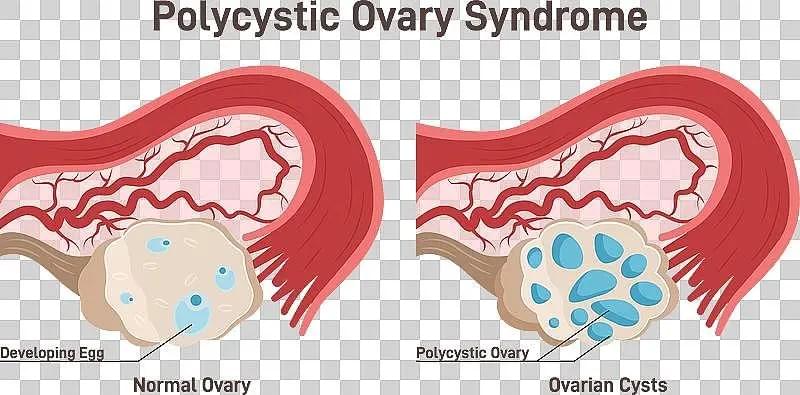
The hallmark of PCOS is the presence of multiple small follicles on the ovaries, visible via ultrasound. However, despite the name “polycystic,” these are not true cysts but immature follicles that fail to mature and release an egg. This lack of ovulation prevents conception from occurring naturally in many cases.
Moreover, insulin resistance—a condition present in up to 70% of women with PCOS—further exacerbates hormonal imbalances. High insulin levels stimulate the ovaries to produce more androgens, which in turn interfere with follicular development and ovulation. This complex interplay between metabolic and reproductive systems underscores the need for a multifaceted treatment approach.
First-Line Treatment: Lifestyle Modifications and Metabolic Optimization
Before initiating medical interventions, healthcare providers typically recommend lifestyle changes as the foundational step in managing PCOS-related infertility. Research consistently shows that even modest weight loss (5–10% of body weight) can restore ovulation and improve fertility outcomes in overweight or obese women with PCOS.
A combination of dietary adjustments, regular physical activity, and behavioral support forms the cornerstone of this approach. Diets emphasizing low glycemic index (GI) foods, balanced macronutrients, and anti-inflammatory properties—such as the Mediterranean diet—have shown particular promise in improving insulin sensitivity and hormonal profiles.
Exercise, particularly moderate-intensity aerobic and resistance training, enhances insulin sensitivity independent of weight loss. Studies indicate that women who engage in at least 150 minutes of moderate exercise per week experience improved menstrual regularity and higher ovulation rates.
Additionally, emerging evidence supports the use of supplements such as inositol (particularly myo-inositol and D-chiro-inositol), which play a role in insulin signaling and follicular maturation. Clinical trials have demonstrated that inositol supplementation can improve ovulation frequency and egg quality, making it a valuable adjunct to lifestyle therapy.
For women with significant insulin resistance, metformin—an oral insulin-sensitizing agent—is often prescribed. While not a fertility drug per se, metformin helps lower insulin and androgen levels, thereby restoring ovulatory function. It is especially beneficial for women with impaired glucose tolerance or prediabetes.
Ovulation Induction: Bridging the Gap to Conception
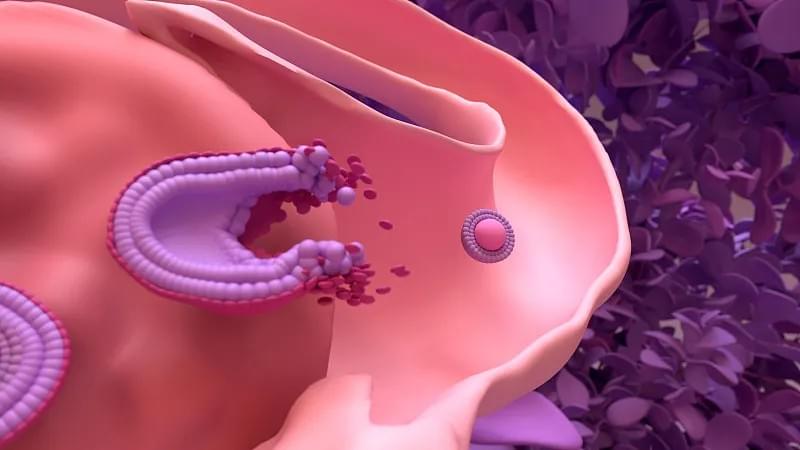
When lifestyle interventions alone are insufficient, ovulation induction (OI) becomes the next step. The goal of OI is to stimulate the ovaries to produce and release a mature egg, thereby increasing the chances of conception.
Clomiphene Citrate (Clomid): For decades, clomiphene citrate has been the first-line pharmacological agent for ovulation induction in PCOS. It works by blocking estrogen receptors in the brain, prompting the pituitary gland to release more follicle-stimulating hormone (FSH), which encourages follicular development.
Typically administered orally for five days early in the menstrual cycle, clomiphene has a success rate of approximately 80% in inducing ovulation, with about 30–40% of women achieving pregnancy within six cycles. However, it may thin the endometrial lining or reduce cervical mucus quality in some patients, potentially affecting implantation.
Letrozole (Femara): In recent years, letrozole—a medication originally developed for breast cancer treatment—has emerged as a superior alternative to clomiphene for ovulation induction in PCOS. Unlike clomiphene, letrozole does not have anti-estrogenic effects on the uterus and cervix, leading to better endometrial development and higher live birth rates.
Multiple randomized controlled trials, including the landmark PPCOS II study, have demonstrated that letrozole results in higher ovulation and pregnancy rates compared to clomiphene, particularly in women with a higher BMI. As a result, many fertility specialists now recommend letrozole as the first-line pharmacological treatment for anovulatory infertility in PCOS.
Advanced Fertility Treatments: When Ovulation Induction Isn't Enough
For women who do not respond to oral medications or fail to conceive after several cycles, more advanced fertility treatments are available.
Gonadotropin Therapy: Injectable gonadotropins (FSH and LH) directly stimulate the ovaries to develop follicles. This treatment is highly effective but requires close monitoring via ultrasound and blood tests to prevent ovarian hyperstimulation syndrome (OHSS), a potentially serious complication more common in women with PCOS due to their high number of follicles.
To mitigate OHSS risk, protocols such as the "step-up" or "step-down" dosing methods are employed. Additionally, the use of a GnRH antagonist during stimulation and triggering ovulation with a GnRH agonist (instead of hCG) can significantly reduce OHSS incidence.
In Vitro Maturation (IVM): IVM is a promising alternative for women with PCOS, especially those at high risk of OHSS. In this technique, immature eggs are retrieved from unstimulated or minimally stimulated ovaries and matured in the laboratory before fertilization. While pregnancy rates with IVM are currently lower than with conventional IVF, ongoing research aims to improve outcomes and make IVM a safer, more accessible option.
In Vitro Fertilization (IVF): IVF remains the most effective treatment for PCOS-related infertility when other methods fail. It involves stimulating the ovaries with gonadotropins, retrieving mature eggs, fertilizing them with sperm in the lab, and transferring the resulting embryo(s) into the uterus.
Modern IVF protocols for PCOS patients emphasize individualized stimulation, meticulous monitoring, and elective single embryo transfer (eSET) to minimize the risk of multiple pregnancies. The use of freeze-all strategies—where all embryos are cryopreserved and transferred in a subsequent cycle—has also improved outcomes by allowing the body to recover from stimulation before implantation, reducing the risk of OHSS and enhancing endometrial receptivity.
Recent advancements in embryo selection, such as preimplantation genetic testing for aneuploidy (PGT-A), may further improve live birth rates, although their routine use in PCOS patients remains a topic of debate due to cost and limited evidence of benefit in this specific population.
Addressing the Emotional and Psychological Dimensions
Infertility, especially when linked to a chronic condition like PCOS, can take a profound emotional toll. Women may experience anxiety, depression, and feelings of isolation, particularly when treatment cycles do not result in pregnancy.
Integrating psychological support into the treatment plan is crucial. Cognitive-behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and peer support groups have been shown to improve emotional well-being and even enhance treatment outcomes. Some studies suggest that reduced stress levels may positively influence hormonal balance and fertility.
Fertility clinics that offer holistic care—combining medical treatment with counseling, nutrition guidance, and mental health support—tend to report higher patient satisfaction and better clinical results. Encouraging open communication between patients and providers fosters trust and empowers women to make informed decisions throughout their fertility journey.
Emerging Therapies and Future Directions
The field of reproductive medicine is rapidly evolving, with several promising therapies on the horizon for PCOS-related infertility.
Laparoscopic Ovarian Drilling (LOD): Once a more common surgical option, LOD involves using a laser or electrocautery to destroy a portion of the ovarian tissue, thereby reducing androgen production and restoring ovulation. While effective in select cases, especially where access to fertility drugs is limited, LOD has largely been replaced by pharmacological treatments due to risks such as adhesion formation and diminished ovarian reserve.
Gut Microbiome Modulation: Emerging research highlights the role of the gut microbiome in metabolic and hormonal regulation. Dysbiosis (imbalance in gut bacteria) has been observed in women with PCOS, and interventions such as probiotics, prebiotics, and dietary fiber may help improve insulin sensitivity and reduce inflammation. While still in early stages, microbiome-targeted therapies could become a complementary strategy in the future.
Personalized Medicine and AI-Driven Protocols: The future of PCOS fertility treatment lies in personalization. Advances in genetic profiling, metabolomics, and artificial intelligence are paving the way for tailored treatment plans based on an individual’s unique hormonal, metabolic, and genetic profile. Machine learning models are being developed to predict ovulation response, optimize drug dosing, and forecast pregnancy outcomes, potentially revolutionizing how we approach infertility care.

Conclusion: A Hopeful Path Forward
PCOS-related infertility is a complex but manageable condition. With a combination of lifestyle optimization, evidence-based medical treatments, and emotional support, most women with PCOS can achieve successful pregnancies. The key lies in early diagnosis, individualized care, and a proactive approach that addresses both the metabolic and reproductive aspects of the syndrome.
As research continues to uncover deeper insights into PCOS pathophysiology and treatment responses, the future holds even greater promise. Women navigating this journey should be reassured that they are not alone—and that with the right guidance and support, the path to parenthood, though sometimes challenging, is very much within reach.
By staying informed and working closely with a multidisciplinary team of healthcare providers, women with PCOS can take control of their fertility and move confidently toward building the families they desire.
