Infertility is a deeply personal and often challenging issue affecting millions of couples worldwide. While discussions around fertility frequently focus on women, male infertility plays a significant role in conception difficulties—accounting for nearly 40-50% of all infertility cases. Despite its prevalence, many men remain unaware of the signs and symptoms that could indicate underlying reproductive health issues. This lack of awareness often delays diagnosis and treatment, reducing the chances of successful intervention.
In this comprehensive guide, we’ll explore the key signs of male infertility, the biological and lifestyle factors that contribute to it, and the importance of early detection. Whether you're trying to conceive or simply interested in men’s reproductive health, understanding these indicators can empower you to take proactive steps toward better health and improved fertility outcomes.
Understanding Male Infertility: The Basics
Before diving into the signs, it's essential to understand what male infertility actually means. Medically, male infertility refers to the inability of a man to cause pregnancy in a fertile female after at least one year of regular, unprotected intercourse. This condition can stem from a variety of factors, including low sperm production, abnormal sperm function, or blockages that prevent the delivery of sperm.
The male reproductive system is a finely tuned mechanism involving the testes, epididymis, vas deferens, prostate gland, and urethra. Any disruption in this system—whether hormonal, structural, or environmental—can impact fertility. Unlike some health conditions with obvious symptoms, male infertility is often silent. Many men do not realize they have fertility issues until they and their partners face challenges in conceiving.
However, certain physical, sexual, and medical signs can serve as red flags. Recognizing these early can lead to timely evaluation by a healthcare provider and potentially more effective treatment options.
Common Physical and Sexual Signs of Male Infertility
While infertility itself may not present with overt symptoms, several physical and sexual indicators can point toward underlying reproductive issues.
1. Changes in Semen Appearance or Volume
One of the most telling signs is a noticeable change in semen. Healthy semen is typically a whitish-gray fluid with a thick consistency that liquefies within 20–30 minutes after ejaculation. If a man observes consistently low semen volume (less than 1.5 milliliters per ejaculation), watery or clear semen, or unusual coloration (such as yellow, green, or blood-tinged), it could indicate a problem with sperm production or delivery.
Low semen volume may be linked to retrograde ejaculation (where semen enters the bladder instead of exiting the penis), blockages in the ejaculatory ducts, or hormonal imbalances. Watery semen often suggests a low sperm count, though it's not a definitive diagnosis on its own.

2. Erectile Dysfunction and Ejaculation Problems
Persistent difficulty achieving or maintaining an erection (erectile dysfunction, or ED) can be both a sexual health concern and a fertility red flag. While ED doesn’t directly cause infertility, it can prevent successful intercourse and sperm delivery. More importantly, ED is often linked to underlying conditions such as low testosterone, diabetes, cardiovascular disease, or psychological stress—all of which can also impair sperm production.
Similarly, premature ejaculation, delayed ejaculation, or painful ejaculation may signal nerve damage, hormonal imbalances, or infections in the reproductive tract. Retrograde ejaculation, where little or no semen is expelled during orgasm, is particularly associated with infertility and may require medical investigation.
3. Testicular Abnormalities
The testes are responsible for producing sperm and testosterone. Any physical changes in the testicles can affect fertility.
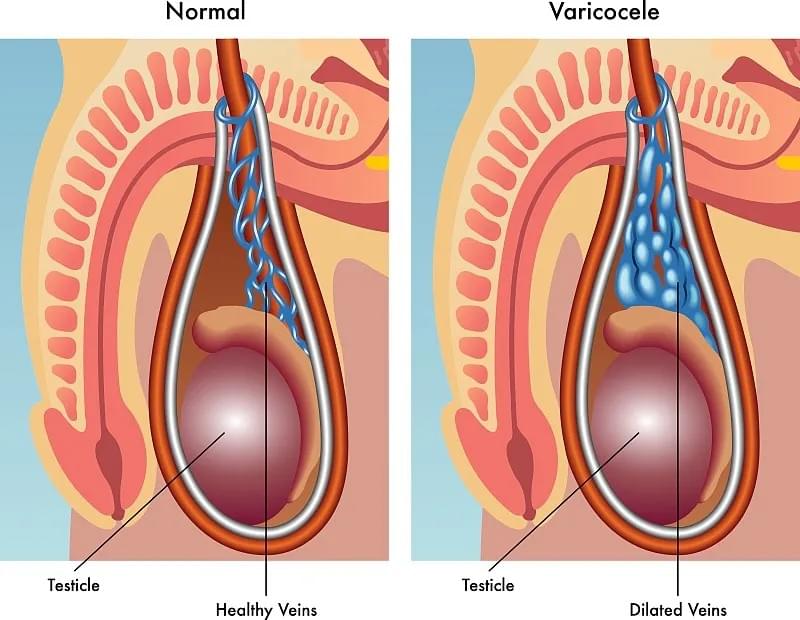
- Varicocele: This is the most common correctable cause of male infertility. A varicocele is an enlargement of the veins within the scrotum, similar to varicose veins in the legs. It can lead to overheating of the testicles, which impairs sperm production and quality. Men with varicoceles may feel a “bag of worms” sensation in the scrotum, especially when standing or straining.
- Undescended Testicles (Cryptorchidism): If one or both testicles fail to descend into the scrotum during fetal development, it can severely impact sperm production later in life.
- Testicular Pain or Swelling: Persistent pain, lumps, or swelling in the testicles may indicate infection (such as epididymitis or orchitis), trauma, or even testicular cancer—all of which can affect fertility.
4. Hormonal Imbalances and Secondary Sexual Characteristics
Hormones like testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) play critical roles in sperm production. When these are out of balance, men may experience physical changes that hint at fertility issues.
Signs of hormonal imbalance include:
- Reduced facial or body hair
- Gynecomastia (enlarged breast tissue in men)
- Decreased muscle mass
- Fatigue or low energy levels
- Loss of libido (sex drive)
These symptoms may point to conditions such as hypogonadism (low testosterone), pituitary gland disorders, or thyroid dysfunction—all of which can impair fertility.
Lifestyle and Environmental Factors That Impact Male Fertility
While biological signs are crucial, it’s equally important to recognize how lifestyle choices and environmental exposures can contribute to infertility.
1. Obesity and Poor Diet
Excess body fat, particularly abdominal fat, increases estrogen levels and lowers testosterone, negatively affecting sperm count and motility. Diets high in processed foods, trans fats, and sugar have been linked to lower sperm quality. Conversely, a diet rich in antioxidants (found in fruits, vegetables, and nuts) supports healthy sperm production.
2. Smoking, Alcohol, and Drug Use
- Smoking: Cigarette smoke contains toxins that damage sperm DNA, reduce sperm count, and impair motility.
- Alcohol: Heavy drinking can lower testosterone levels and lead to liver damage, both of which affect fertility.
- Recreational Drugs: Anabolic steroids, marijuana, and cocaine have all been shown to disrupt hormone levels and sperm production.
3. Heat Exposure and Toxins
The testes function best at a temperature slightly below body temperature. Prolonged exposure to heat—such as from hot tubs, saunas, tight underwear, or sitting for long periods—can raise scrotal temperature and reduce sperm production.
Additionally, exposure to environmental toxins like pesticides, heavy metals (lead, mercury), and industrial chemicals (BPA, phthalates) can impair reproductive health.

Medical Conditions Linked to Male Infertility
Certain pre-existing medical conditions are strongly associated with reduced fertility.
1. Infections
Infections of the reproductive tract, such as sexually transmitted infections (STIs) like chlamydia or gonorrhea, can cause scarring and blockages in the sperm-carrying tubes. Other infections, such as mumps orchitis (mumps affecting the testicles), can permanently damage testicular tissue.
2. Genetic Disorders
Some genetic conditions directly impact fertility:
- Klinefelter Syndrome: Men with an extra X chromosome (XXY) often have small testes and produce little or no sperm.
- Y Chromosome Microdeletions: Missing genes on the Y chromosome can impair sperm production.
- Cystic Fibrosis: While rare, men with cystic fibrosis may be born without the vas deferens, the tube that carries sperm.
3. Chronic Illnesses
Diabetes, kidney disease, and autoimmune disorders can all interfere with hormonal balance and sperm function. For example, diabetic neuropathy can lead to retrograde ejaculation.
When to Seek Medical Evaluation
If you and your partner have been trying to conceive for over a year (or six months if the female partner is over 35), it’s time to seek a fertility evaluation. However, you don’t need to wait that long if you notice any of the following:
- A history of testicular, prostate, or sexual health issues
- Previous surgeries in the groin or pelvic area
- Exposure to chemotherapy or radiation
- Family history of fertility problems
A basic male fertility assessment typically includes:
- Semen Analysis: The cornerstone of male fertility testing, evaluating sperm count, motility, morphology (shape), and volume.
- Hormone Testing: Blood tests to check testosterone, FSH, LH, and other hormone levels.
- Physical Examination: To detect varicoceles, testicular abnormalities, or signs of hormonal imbalance.
- Ultrasound or Genetic Testing: If initial tests are inconclusive, further imaging or DNA analysis may be recommended.
Treatment and Fertility Preservation Options
The good news is that many causes of male infertility are treatable. Depending on the diagnosis, treatment options may include:
- Surgery: To correct varicoceles or repair blocked ducts.
- Hormone Therapy: To address imbalances in testosterone or other reproductive hormones.
- Antibiotics: To treat infections affecting the reproductive tract.
- Assisted Reproductive Technologies (ART): Such as intrauterine insemination (IUI) or in vitro fertilization (IVF) with intracytoplasmic sperm injection (ICSI), which can help even men with very low sperm counts achieve fatherhood.
For men undergoing cancer treatment or facing other fertility-threatening conditions, sperm banking (cryopreservation) offers a way to preserve fertility for the future.

Breaking the Stigma: Mental Health and Male Fertility
Infertility can take a significant emotional toll. Men often feel a sense of failure, shame, or inadequacy, especially in cultures where masculinity is closely tied to virility. This emotional burden can lead to anxiety, depression, and relationship strain.
It’s crucial to recognize that infertility is a medical condition—not a personal failing. Open communication with partners, seeking counseling, and joining support groups can help men navigate the emotional challenges of infertility.
Healthcare providers also play a key role in creating a supportive environment where men feel comfortable discussing their concerns without judgment.
Conclusion: Early Awareness Leads to Better Outcomes
Male infertility is more common than many realize, yet it remains under-discussed and often misunderstood. By recognizing the signs—whether physical, sexual, or lifestyle-related—men can take control of their reproductive health earlier and seek appropriate care.
If you suspect fertility issues, don’t wait. Early evaluation leads to better treatment outcomes and increases the chances of building the family you desire. With advances in medical science and growing awareness, there is real hope for couples facing infertility.
By sharing accurate, science-based information like this, we aim to reduce stigma, promote early detection, and support men on their journey to fatherhood.
