Surrogacy has revolutionized the way families are built, offering hope to individuals and couples facing infertility, genetic disorders, or other reproductive challenges. As assisted reproductive technology (ART) continues to evolve, one of the most significant advancements enhancing the success and safety of surrogacy is Pre-implantation Genetic Testing (PGT). This powerful diagnostic tool allows prospective parents and fertility specialists to select embryos free from specific genetic abnormalities before implantation, significantly increasing the chances of a healthy pregnancy and baby.
In this comprehensive guide, we’ll explore the role of PGT in surrogacy, how it works, its benefits, ethical considerations, and why it’s becoming an essential component of modern fertility treatments. Whether you're considering surrogacy, already in the process, or simply seeking to understand the science behind it, this article will provide valuable insights into one of the most transformative developments in reproductive medicine.
What Is Pre-implantation Genetic Testing (PGT)?
Pre-implantation Genetic Testing (PGT) is a laboratory procedure used during in vitro fertilization (IVF) to analyze embryos for genetic abnormalities before they are transferred to the uterus. In the context of surrogacy, this means that embryos created from the intended parents’ (or donors’) eggs and sperm can be screened for chromosomal or genetic issues prior to being implanted into the surrogate mother.
PGT was formerly known as Pre-implantation Genetic Diagnosis (PGD) and Pre-implantation Genetic Screening (PGS), but the terminology has been standardized by the International Committee Monitoring Assisted Reproductive Technologies (ICMART) and the American Society for Reproductive Medicine (ASRM) to reflect the different types of testing more accurately:
- PGT-A (Aneuploidy Screening): Detects abnormalities in chromosome number (e.g., missing or extra chromosomes), such as those seen in Down syndrome.
- PGT-M (Monogenic/Single Gene Disorders): Screens for specific inherited genetic conditions like cystic fibrosis, sickle cell anemia, or Huntington’s disease.
- PGT-SR (Structural Rearrangements): Used when one or both parents carry chromosomal rearrangements (e.g., translocations) that could lead to unbalanced embryos.
By identifying genetically healthy embryos, PGT helps reduce the risk of miscarriage, failed implantation, and the birth of children with serious genetic conditions.
How PGT Works in the Surrogacy Process
The integration of PGT into surrogacy involves a coordinated sequence of steps that begin long before the embryo transfer. Here’s how it typically unfolds:
- Ovarian Stimulation and Egg Retrieval: The intended mother or egg donor undergoes hormonal stimulation to produce multiple mature eggs. These eggs are then retrieved through a minor surgical procedure.
- Fertilization via IVF: The eggs are fertilized with sperm from the intended father or a donor in a laboratory setting, creating embryos.
- Embryo Culture: The embryos are cultured for 5–6 days until they reach the blastocyst stage, which provides enough cells for accurate genetic testing.
- Biopsy: A few cells are carefully extracted from the trophectoderm (the part of the blastocyst that will become the placenta) without harming the inner cell mass (which becomes the fetus).
- Genetic Analysis: The biopsied cells are sent to a specialized genetics lab for PGT-A, PGT-M, or PGT-SR analysis, depending on the clinical indication.
- Results and Embryo Selection: Within 7–14 days, results are returned, indicating which embryos are genetically normal or unaffected by the condition being tested.
- Embryo Transfer: A genetically healthy embryo is selected and transferred into the surrogate’s uterus during a synchronized cycle.
- Pregnancy Confirmation: A blood test about 10–14 days after transfer confirms whether implantation was successful.
This meticulous process ensures that only the healthiest embryos are used, maximizing the chances of a successful surrogacy journey.

Why PGT Is Especially Valuable in Surrogacy
While PGT is beneficial in any IVF cycle, its advantages are particularly pronounced in surrogacy arrangements. Here’s why:
1. Higher Success Rates
One of the leading causes of IVF failure is chromosomal abnormalities in embryos. By selecting euploid (chromosomally normal) embryos, PGT-A significantly improves implantation rates and reduces miscarriage risk. For surrogates—often chosen for their proven fertility—PGT ensures that the embryo, not the uterine environment, is optimized for success.
Studies show that PGT-A can increase live birth rates per transfer by up to 20% in certain patient groups, especially women over 35 or those with a history of recurrent pregnancy loss.
2. Reduced Emotional and Physical Burden on the Surrogate
Surrogates commit to carrying a child for someone else, often undergoing hormone therapy and medical procedures. Using PGT minimizes the risk of transferring an embryo that may not implant or could result in a miscarriage, thereby reducing the number of transfer cycles and emotional strain on the surrogate.
3. Prevention of Inherited Genetic Diseases
For intended parents with a known family history of genetic disorders, PGT-M offers a powerful way to prevent passing on conditions like Tay-Sachs disease, spinal muscular atrophy, or BRCA mutations. This is especially critical when both partners are carriers of recessive disorders.
4. Informed Decision-Making
PGT provides clear, actionable data. Intended parents can make informed choices about which embryos to transfer, freeze, or discard. This transparency fosters confidence and reduces anxiety during the surrogacy process.
5. Fewer Multiple Pregnancies
Without PGT, clinics may transfer multiple embryos to increase the odds of success, raising the risk of twins or triplets. With PGT, a single euploid embryo transfer (SET) becomes a viable and safer option, reducing complications for both the surrogate and the baby.
Who Should Consider PGT in Surrogacy?
While PGT is not mandatory, it is strongly recommended for certain individuals and couples:
- Advanced Maternal Age (35+): Egg quality declines with age, increasing the risk of aneuploidy.
- Recurrent Miscarriages: Often linked to chromosomal abnormalities.
- Repeated IVF Failure: Suggests possible embryonic issues.
- Known Genetic Carriers: Individuals with a family history or confirmed carrier status for monogenic disorders.
- Balanced Chromosomal Translocation Carriers: At risk of producing unbalanced embryos.
- Same-Sex Male Couples Using Donor Eggs: To ensure the highest quality embryo selection when building their family through surrogacy.
Even for those without known risk factors, many fertility specialists recommend PGT-A as a proactive measure to improve outcomes.
Addressing Common Misconceptions About PGT
Despite its benefits, PGT is sometimes misunderstood. Let’s clarify a few common myths:
Myth 1: PGT Guarantees a Healthy Baby
While PGT greatly reduces the risk of certain genetic conditions, it does not eliminate all potential health issues. Prenatal testing (e.g., NIPT, amniocentesis) is still recommended during pregnancy to confirm fetal health.
Myth 2: PGT Harms the Embryo
Modern biopsy techniques are highly refined. When performed by experienced embryologists, the procedure poses minimal risk to embryo viability. Studies show no significant difference in birth defect rates between PGT and non-PGT babies.
Myth 3: PGT Is Only for Older Women
While age is a major factor, younger patients with genetic risks or recurrent loss can also benefit significantly.
Myth 4: PGT Leads to “Designer Babies”
PGT is strictly used to screen for serious medical conditions, not to select for traits like intelligence, height, or eye color. Ethical guidelines and regulations strictly prohibit non-medical embryo selection in most countries.
Ethical and Legal Considerations
The use of PGT in surrogacy raises important ethical and legal questions that vary by jurisdiction.
Embryo Disposition
What happens to embryos identified as abnormal or unused? Options include donation to research, thawing without transfer, or indefinite freezing. Intended parents should discuss these decisions with their clinic and legal advisors in advance.
Genetic Privacy
Genetic data is sensitive. Clinics and labs must comply with data protection laws (e.g., GDPR in Europe, HIPAA in the U.S.) to ensure confidentiality.
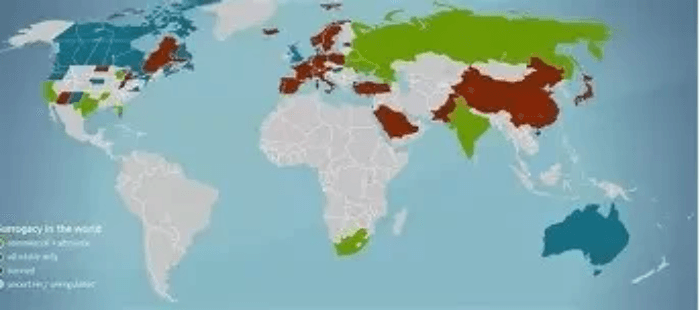
Regulatory Landscape
Countries differ widely in their PGT regulations. For example:
- The U.S. allows broad use of PGT with minimal federal restrictions.
- The UK permits PGT only for serious genetic conditions, approved by the HFEA.
- Germany restricts embryo biopsy and genetic testing under its Embryo Protection Act.
Intended parents pursuing international surrogacy must understand the legal framework of both the surrogacy destination and their home country.
The Role of Fertility Clinics and Genetic Counselors
A successful PGT-enabled surrogacy journey requires a multidisciplinary team:
- Reproductive Endocrinologists (REs): Oversee the IVF and surrogacy process.
- Embryologists: Perform egg retrieval, fertilization, biopsy, and embryo culture.
- Genetic Counselors: Help intended parents understand test results, inheritance risks, and implications.
- Surrogacy Agencies: Coordinate logistics, legal contracts, and surrogate care.
- Psychologists: Provide emotional support throughout the process.
Genetic counseling is especially crucial before PGT-M. Counselors help couples understand carrier status, the probability of affected embryos, and the emotional impact of potential results.
Case Study: A Real-World Example
Consider the case of a heterosexual couple in their late 30s who had experienced three miscarriages. Genetic testing revealed that both were carriers of spinal muscular atrophy (SMA), a life-threatening neuromuscular disorder. They opted for surrogacy with PGT-M.
After IVF, 8 embryos were created. PGT-M analysis showed that 3 were unaffected, 2 were carriers (but healthy), and 3 were affected by SMA. One unaffected embryo was transferred to their surrogate, resulting in a successful pregnancy and the birth of a healthy baby girl.
Without PGT, the couple faced a 25% chance of having an affected child with each pregnancy. PGT allowed them to avoid passing on the disease and achieve a healthy outcome.
Advances in PGT Technology
The field of genetic testing is rapidly advancing. Newer technologies are improving the accuracy, speed, and scope of PGT:
- Next-Generation Sequencing (NGS): Offers higher resolution and more detailed analysis than older methods like FISH or aCGH.
- Comprehensive Chromosome Screening (CCS): Evaluates all 24 chromosomes for aneuploidy.
- Polygenic Risk Scoring (Emerging): Still experimental, this could one day assess risk for complex conditions like diabetes or heart disease—but raises significant ethical concerns.
These innovations promise even better outcomes in the future, though they must be balanced with ethical oversight.

Cost and Accessibility
PGT adds to the overall cost of surrogacy, typically ranging from 3,000 to 7,000 depending on the type of testing and number of embryos. While this may seem high, many intended parents view it as a worthwhile investment given the potential to avoid failed cycles, miscarriages, or the birth of a child with a severe condition.
Insurance coverage varies. In the U.S., some plans cover PGT for medical indications (e.g., known genetic disorders), but not for elective use. International patients often seek treatment in countries like Spain, Greece, or Mexico, where costs are lower and regulations more favorable.
Looking Ahead: The Future of PGT in Surrogacy
As genetic science progresses, PGT is likely to become even more integrated into standard surrogacy protocols. We may see:
- Non-Invasive PGT (niPGT): Analyzing genetic material shed by the embryo into the culture medium, eliminating the need for biopsy.
- Artificial Intelligence (AI) in Embryo Selection: Combining PGT data with time-lapse imaging to predict embryo viability with greater accuracy.
- Expanded Carrier Screening: Routine testing for hundreds of genetic conditions before IVF begins.
However, these advances must be guided by ethical principles, patient autonomy, and equitable access.

Conclusion
Pre-implantation Genetic Testing (PGT) has transformed surrogacy from a hopeful endeavor into a more predictable and secure path to parenthood. By enabling the selection of genetically healthy embryos, PGT enhances success rates, reduces risks, and empowers intended parents to make informed decisions.
Whether you're concerned about age-related fertility decline, have a family history of genetic disease, or simply want to maximize your chances of a healthy baby, PGT offers a powerful tool within the surrogacy journey. As technology continues to evolve, the integration of genetics and reproductive medicine will only deepen, offering new hope to families worldwide.
If you're considering surrogacy, speak with a fertility specialist and genetic counselor to determine whether PGT is right for your unique situation. With the right support and advanced science, your dream of building a family can become a reality.
