Surrogacy is a deeply meaningful journey for intended parents and surrogates alike — a path that allows families to be built where traditional conception may not be possible. At the heart of this process lies medical science, particularly reproductive endocrinology, which ensures that every step from embryo transfer to successful implantation is supported by precise hormonal regulation. Among the most critical components of a successful surrogacy cycle are hormonal treatments, which prepare the surrogate’s body to receive and nurture an embryo.
For individuals and couples exploring surrogacy options, understanding the role of hormones is essential. Not only does it demystify the medical process, but it also empowers all parties involved with knowledge, reducing anxiety and fostering informed decision-making. This article dives into the science, protocols, benefits, and considerations surrounding hormonal treatments in surrogacy, offering valuable insights for intended parents, surrogates, and healthcare professionals navigating this field.
Why Hormonal Treatments Are Essential in Surrogacy
In natural conception, a woman’s menstrual cycle is governed by a delicate balance of hormones such as estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). These regulate ovulation, uterine lining development, and pregnancy maintenance. However, in gestational surrogacy — where the surrogate carries an embryo created from the intended parents’ or donors’ genetic material — there is no natural ovulation involved. Therefore, the surrogate’s body must be medically prepared to support embryo implantation and early fetal development.
This preparation hinges on hormone replacement therapy (HRT), which mimics the natural hormonal environment required for pregnancy. Without proper hormonal synchronization between the embryo’s developmental stage and the surrogate’s uterine receptivity, implantation failure or early miscarriage can occur.
Hormonal treatment ensures:
- The uterine lining (endometrium) reaches optimal thickness and texture for implantation.
- The timing of embryo transfer aligns perfectly with peak receptivity.
- Early pregnancy support is maintained until the placenta takes over hormone production.
These treatments are typically administered over several weeks leading up to and following embryo transfer, under close medical supervision.

The Hormones Involved: Estrogen, Progesterone, and More
The two primary hormones used in surrogacy cycles are estrogen and progesterone. Each plays a distinct and vital role in preparing and maintaining the uterine environment.
1. Estrogen: Building the Foundation
Estrogen is responsible for stimulating the growth of the endometrial lining. In a typical cycle, rising estrogen levels thicken the uterine wall after menstruation, creating a nutrient-rich environment ready for embryo attachment.
In surrogacy, synthetic estrogen is introduced externally through various forms:
- Oral tablets (e.g., estradiol)
- Transdermal patches applied to the skin
- Vaginal gels or suppositories
The method chosen depends on the clinic’s protocol and the surrogate’s individual response. Transdermal patches are often preferred because they provide steady absorption and avoid first-pass liver metabolism, potentially reducing side effects like nausea or blood clot risk.
Treatment usually begins shortly after confirming the surrogate has no active ovarian function (often achieved via birth control pills or GnRH agonists beforehand). Over 10–14 days, regular ultrasounds monitor endometrial thickness. An ideal lining measures between 8–12 mm, with a triple-line pattern indicating high receptivity.
2. Progesterone: Sealing the Environment for Implantation
Once the endometrium is sufficiently developed, progesterone is introduced. This hormone transforms the thickened lining into a secretory state — rich in glands and blood vessels — capable of supporting embryo implantation and early placental development.
Progesterone administration typically starts 5–6 days before the planned embryo transfer and continues well into the first trimester. Methods include:
- Intramuscular (IM) injections – Most common; highly effective but can cause discomfort or bruising.
- Vaginal suppositories or gels – Less invasive, though some report leakage or irritation.
- Subcutaneous injections – Newer option, offering ease of use with fewer side effects than IM.
Recent studies suggest that combining vaginal and injectable forms may improve outcomes, especially in cases with prior implantation failure.
3. Supportive Medications: hCG, LH, and Others
While estrogen and progesterone form the backbone of hormonal treatment, other medications may be used adjunctively:
- Human chorionic gonadotropin (hCG): Sometimes used to trigger final endometrial maturation.
- Low-dose aspirin or heparin: Prescribed in cases of suspected clotting disorders to improve blood flow to the uterus.
- Corticosteroids (e.g., prednisone): Occasionally used to modulate immune response, though evidence remains debated.
All medications are tailored to the surrogate’s health profile, previous cycle responses, and embryology lab recommendations.
The Typical Hormonal Protocol Timeline
Understanding the timeline helps both intended parents and surrogates anticipate what to expect. While protocols vary slightly between clinics, a standard schedule looks like this:
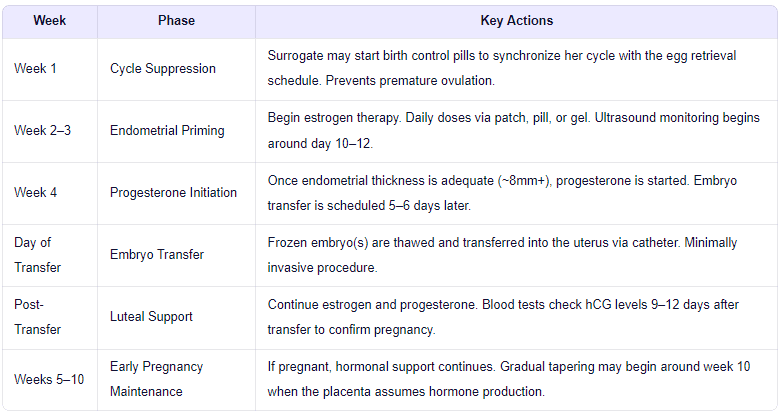
It's important to note that frozen embryo transfers (FET) are now more common than fresh transfers in surrogacy due to better synchronization and higher success rates. FET allows full control over the hormonal environment without relying on the surrogate’s natural cycle.
Moreover, personalized dosing based on bloodwork (measuring estradiol and progesterone levels) ensures each surrogate receives the right amount — avoiding under- or over-stimulation.
Benefits of Hormonal Treatments in Surrogacy
When properly administered, hormone therapy significantly enhances the chances of a successful surrogacy journey. Key benefits include:
✅ Improved Uterine Receptivity
By precisely controlling hormone levels, clinicians can optimize the “window of implantation” — the brief period when the endometrium is most receptive to an embryo. Studies show that synchronized HRT cycles yield implantation rates of 50–60% and clinical pregnancy rates exceeding 60% per transfer in experienced clinics.
✅ Flexibility and Coordination
Hormonal protocols allow perfect timing between embryo availability (from IVF cycles) and the surrogate’s readiness. This is especially valuable when using donor eggs or when intended parents need time to complete genetic testing.
✅ Reduced Risk of Early Loss
Consistent progesterone support prevents luteal phase deficiency, a condition linked to early miscarriage. Maintaining stable hormone levels in the first 8–10 weeks reduces the risk of biochemical pregnancies and spontaneous abortion.
✅ Greater Predictability
Unlike natural cycles, which can vary month to month, artificial cycles offer consistency. This predictability improves planning for travel, legal procedures, and emotional preparation.
Potential Side Effects and Management Strategies
While generally safe, hormonal treatments can cause side effects. Most are mild and manageable, but awareness and proactive care are crucial.
Common Side Effects:
- Bloating and breast tenderness (due to high estrogen)
- Mood swings or fatigue
- Headaches or mild nausea
- Injection site pain or bruising (especially with IM progesterone)
Less Common but Important Risks:
- Ovarian hyperstimulation syndrome (OHSS): Rare in surrogates since they aren’t undergoing ovarian stimulation, but possible if residual follicular activity exists.
- Blood clots: Estrogen increases clotting risk slightly; patients with thrombophilia may require anticoagulants.
- Allergic reactions: To ingredients in vaginal formulations or adhesives in patches.
Clinics mitigate risks through:
- Routine blood testing to monitor hormone levels.
- Using transdermal or subcutaneous routes to minimize peak serum concentrations.
- Educating surrogates on warning signs (e.g., severe abdominal pain, shortness of breath).
Open communication between the surrogate, coordinator, and medical team ensures any concerns are addressed promptly.

Innovations and Future Directions in Hormonal Support
As reproductive medicine advances, so do the tools and techniques for optimizing hormonal support in surrogacy.
🔬 Personalized Dosing Algorithms
Some clinics now use pharmacokinetic modeling to tailor estrogen and progesterone doses based on a woman’s weight, metabolism, and prior response. This precision approach minimizes side effects and maximizes efficacy.
🧪 Vaginal Micronized Progesterone (VMP) Enhancements
New delivery systems, such as bioadhesive gels and sustained-release inserts, improve retention and absorption, reducing the need for multiple daily applications.
📱 Digital Monitoring Tools
Wearable devices and mobile apps allow real-time tracking of symptoms, medication adherence, and even temperature fluctuations. Some integrate with clinic portals for seamless data sharing.
🌿 Natural Cycle and Minimal Stimulation Approaches
Though less common in surrogacy, some programs explore modified natural cycles where the surrogate’s own ovulation is monitored and supplemented lightly with progesterone. These aim to mimic physiology more closely but require tighter scheduling and carry higher cancellation risks.
Research continues into biomarkers of receptivity, such as the Endometrial Receptivity Array (ERA) test, which analyzes gene expression to pinpoint the ideal transfer window. While controversial due to mixed study results, it represents a move toward truly individualized care.
Emotional and Psychological Considerations
Hormonal treatments don’t just affect the body — they influence mood and emotional well-being. Surrogates often experience heightened emotions due to elevated hormone levels, compounded by the psychological weight of carrying someone else’s child.
Intended parents may also feel anxious during the waiting period post-transfer, commonly known as the “two-week wait.” Clear communication, counseling, and strong support networks are vital.
Best practices include:
- Providing mental health resources throughout the journey.
- Encouraging journaling or mindfulness practices.
- Facilitating regular check-ins between surrogates and coordinators.
Empathy, transparency, and emotional intelligence are just as important as medical expertise in achieving a positive outcome.

Conclusion: Hormones as the Bridge to Parenthood
Hormonal treatments in surrogacy are far more than a medical necessity — they represent the scientific bridge between intention and reality. By carefully orchestrating estrogen and progesterone levels, fertility specialists create the ideal internal environment for life to take root.
For intended parents, understanding these processes fosters trust and reduces uncertainty. For surrogates, it highlights the incredible physiological contribution they make — one that goes beyond genetics to include nurturing at the most fundamental biological level.
As technology evolves and personalization becomes standard, the success and safety of hormonal protocols will continue to improve. Yet, the core remains unchanged: a profound collaboration between science, compassion, and human willpower.
If you're considering surrogacy — whether as an intended parent or a potential surrogate — engaging with a reputable clinic that prioritizes both medical excellence and emotional support is key. Ask questions, understand your protocol, and know that every injection, every ultrasound, and every blood test brings you one step closer to building a family.
Are you ready to explore your surrogacy journey? Contact our international surrogacy coordination team today for a free consultation and personalized guidance on hormonal preparation, legal frameworks, and global program options.
