In the ever-evolving landscape of reproductive medicine, few advancements have had as profound an impact as embryo transfer technology. Once a concept confined to the realm of science fiction, the ability to fertilize an embryo outside the human body and successfully implant it into the uterus has become a cornerstone of modern fertility treatments. Today, embryo transfer stands at the forefront of assisted reproductive technologies (ART), offering hope to millions of individuals and couples struggling with infertility. This article explores the science behind embryo transfer, its various techniques, recent technological innovations, and what the future holds for this transformative medical field.
Understanding Embryo Transfer: A Foundational Overview
Embryo transfer is the final and critical step in the in vitro fertilization (IVF) process. It involves placing a developing embryo into a woman’s uterus with the goal of achieving a successful pregnancy. The journey begins with ovarian stimulation, where fertility medications are used to encourage the ovaries to produce multiple mature eggs. These eggs are then retrieved and combined with sperm in a laboratory setting—a process known as fertilization. After successful fertilization, the resulting embryos are cultured and monitored for several days to assess their development and viability.
The transfer itself is a minimally invasive procedure typically performed without anesthesia. Using a thin, flexible catheter, a trained embryologist or reproductive specialist gently places one or more embryos into the uterine cavity. The timing of the transfer is crucial and is usually scheduled between three to five days after egg retrieval, depending on the embryo’s stage of development.

Types of Embryo Transfer: Tailoring Treatment to Individual Needs
Not all embryo transfers are the same. Medical professionals utilize different approaches based on patient history, embryo quality, and reproductive goals. The two primary types are fresh embryo transfer and frozen embryo transfer (FET).
Fresh Embryo Transfer involves transferring an embryo into the uterus during the same cycle in which the eggs were retrieved. While this method allows for a quicker timeline, it may not always be the optimal choice, especially if hormonal levels are elevated post-stimulation, which can affect uterine receptivity.
Frozen Embryo Transfer (FET), on the other hand, has gained significant popularity in recent years. In this approach, embryos are cryopreserved using vitrification—a rapid freezing technique that prevents ice crystal formation and preserves embryo integrity. The transfer is then performed in a subsequent cycle, often when the woman’s hormonal environment is more favorable. Studies have shown that FET can lead to higher implantation rates and lower risks of complications such as ovarian hyperstimulation syndrome (OHSS).
Additionally, single embryo transfer (SET) is increasingly recommended to reduce the risk of multiple pregnancies, which carry higher health risks for both mother and babies. With advancements in embryo selection and culture techniques, SET is proving to be just as effective as transferring multiple embryos, but with improved safety outcomes.
Technological Innovations Driving Success Rates
The success of embryo transfer is not solely dependent on the transfer procedure itself but also on the technologies used to support embryo development and selection. Over the past decade, several innovations have significantly improved pregnancy rates and patient outcomes.
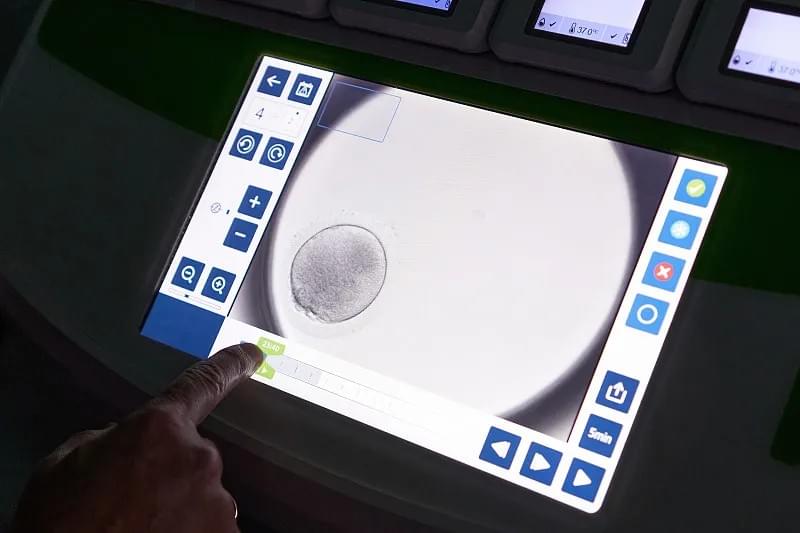
One of the most notable advancements is time-lapse imaging. This technology allows continuous monitoring of embryo development without removing them from the incubator. By capturing images at regular intervals, embryologists can assess morphological changes and identify the most viable embryos based on dynamic growth patterns. This non-invasive method enhances selection accuracy and reduces the need for invasive genetic testing in some cases.
Another groundbreaking development is preimplantation genetic testing (PGT). PGT enables the screening of embryos for chromosomal abnormalities (PGT-A), single-gene disorders (PGT-M), and structural rearrangements (PGT-SR). By transferring only genetically normal embryos, clinics can increase the likelihood of a healthy pregnancy and reduce the risk of miscarriage.
The Role of Artificial Intelligence in Embryo Selection
Artificial intelligence (AI) is beginning to play a transformative role in embryo transfer technology. Machine learning algorithms are being trained on vast datasets of embryo images and developmental outcomes to predict which embryos have the highest potential for implantation. These AI-powered tools assist embryologists by providing objective, data-driven insights that complement human expertise.
For example, AI can analyze subtle morphological features that may be imperceptible to the human eye, such as cell symmetry, fragmentation patterns, and cleavage timing. When integrated into clinical workflows, AI enhances decision-making and contributes to more personalized treatment plans.
While AI is not intended to replace skilled embryologists, it serves as a powerful augmentation tool, helping to standardize embryo evaluation across different clinics and reduce subjectivity in the selection process.
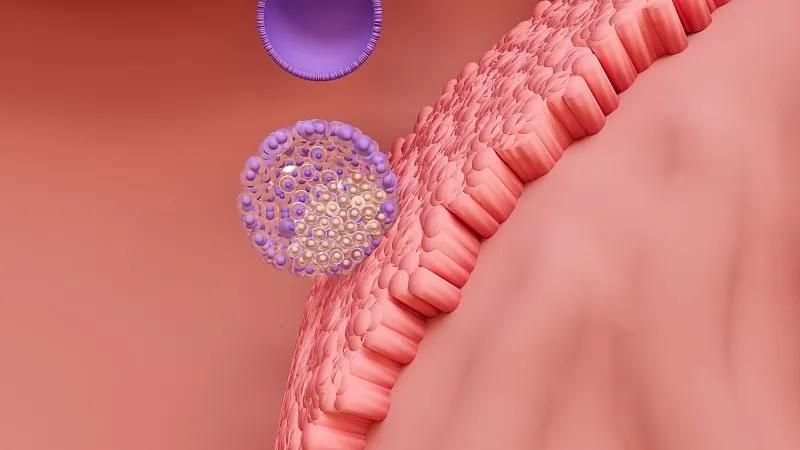
Improving Uterine Receptivity: The Other Half of the Equation
While much attention is given to embryo quality, the success of transfer also hinges on uterine receptivity—the uterus’s ability to accept and support an implanting embryo. Researchers are now focusing on optimizing the endometrial environment through advanced diagnostics and personalized hormone regimens.
Techniques such as endometrial receptivity analysis (ERA) involve taking a biopsy of the uterine lining to determine the optimal window for implantation. This personalized approach ensures that the embryo is transferred when the endometrium is most receptive, thereby increasing the chances of successful implantation.
Ethical and Global Considerations
As embryo transfer technology advances, it also raises important ethical and regulatory questions. Issues such as embryo freezing duration, the disposal of unused embryos, and access to fertility treatments vary widely across countries. In some regions, strict regulations limit the number of embryos that can be created or transferred, while others offer more liberal frameworks.
Moreover, the high cost of IVF and embryo transfer remains a barrier for many individuals. Efforts to improve affordability and insurance coverage are essential to ensure equitable access to these life-changing technologies.
The Future of Embryo Transfer: Toward Greater Precision and Accessibility
Looking ahead, the future of embryo transfer technology is poised for even greater innovation. Scientists are exploring in vitro gametogenesis (IVG)—the creation of eggs and sperm from stem cells—which could revolutionize fertility treatment for individuals who cannot produce their own gametes. Additionally, advances in womb simulation technology and artificial uterine environments may one day allow embryos to develop entirely outside the human body, although this remains in the experimental stage.
Another promising frontier is the integration of multi-omics data—combining genomics, transcriptomics, and metabolomics—to create a comprehensive profile of embryo health. This holistic approach could further refine selection criteria and improve success rates.

Conclusion
Embryo transfer technology has come a long way since the birth of the first IVF baby in 1978. Today, it represents a sophisticated blend of biology, engineering, and data science, offering renewed hope to those facing fertility challenges. As research continues to unravel the complexities of early human development, we can expect even more precise, effective, and accessible treatments in the years to come.
For clinics and healthcare providers, staying at the cutting edge of embryo transfer technology is not just a matter of medical excellence—it is a commitment to improving lives. By embracing innovation and ethical practice, the global fertility community can continue to expand the boundaries of what is possible in reproductive medicine.
Whether you are a patient exploring your options or a medical professional seeking to deepen your understanding, the evolution of embryo transfer technology is a testament to human ingenuity and the enduring desire to build families.
