Surrogacy offers a beacon of hope for countless individuals and couples facing infertility, medical conditions, or other barriers to biological parenthood. As assisted reproductive technologies (ART) advance and societal acceptance grows, more people are turning to surrogacy as a viable path to building families. However, one of the most significant yet often overlooked hurdles in this journey is securing adequate insurance coverage. Despite its growing prevalence, insurance for surrogacy remains fraught with challenges, inconsistencies, and glaring gaps—leaving intended parents, surrogates, and even healthcare providers navigating a complex and uncertain financial landscape.
This article delves into the current state of insurance coverage for surrogacy, examining the systemic obstacles, regional disparities, ethical dilemmas, and financial risks involved. We’ll also explore potential solutions and strategies for stakeholders seeking to improve access and affordability in this critical area of reproductive healthcare.
The Growing Demand for Surrogacy and the Insurance Gap
In recent years, global demand for surrogacy has surged. According to data from the Society for Assisted Reproductive Technology (SART), over 3,000 gestational carrier cycles were reported in the United States alone in 2022—an increase of nearly 40% compared to a decade earlier. This rise is driven by factors such as delayed childbearing, rising infertility rates, and greater recognition of LGBTQ+ family-building rights.
Yet, despite increasing utilization, insurance systems have not kept pace. Most standard health insurance plans—both employer-sponsored and individual policies—either explicitly exclude surrogacy-related services or offer only partial coverage. Even in countries with universal healthcare, such as Canada and the UK, public funding rarely extends to cover the full spectrum of surrogacy costs, including IVF procedures, legal fees, psychological evaluations, and surrogate compensation.

Common Insurance Exclusions and Policy Limitations
One of the primary challenges lies in how insurance policies define and categorize surrogacy. Many insurers classify it as an elective or non-essential procedure rather than a medically necessary fertility treatment. This misclassification leads to widespread exclusions across several key areas:
1. Fertility Treatments and IVF Cycles
In vitro fertilization (IVF), a foundational step in gestational surrogacy, is often only partially covered—or not at all—by insurance. In the U.S., only 19 states mandate some level of IVF coverage, and even within those states, restrictions apply. For example, policies may limit the number of embryo transfers or exclude medication costs, which can exceed $10,000 per cycle.
Moreover, when IVF is performed specifically for surrogacy purposes, many insurers deny coverage outright, arguing that the procedure benefits the intended parents rather than the insured individual (the surrogate). This creates a Catch-22: the surrogate carries the pregnancy, but her policy typically won’t cover the IVF process used to create the embryo.
2. Maternity Care for Surrogates
While most insurance plans cover standard prenatal and delivery care, complications arise when the pregnant individual is acting as a gestational carrier. Some insurers refuse to pay for maternity services if they discover the pregnancy resulted from a surrogacy arrangement, citing policy exclusions for “non-traditional” pregnancies.
Additionally, pre-existing condition clauses and lack of proper rider agreements can leave surrogates vulnerable. If a surrogate develops gestational diabetes, preeclampsia, or requires a cesarean section, out-of-pocket expenses could become overwhelming—especially if her insurer later disputes coverage based on undisclosed surrogacy status.
3. Newborn and Neonatal Coverage
Another critical gap involves neonatal care. In cases of premature birth or congenital abnormalities, newborns may require extended hospital stays in neonatal intensive care units (NICUs), costing tens or even hundreds of thousands of dollars. While intended parents are biologically related to the child, their insurance may not automatically extend to the baby until after legal parentage is established post-birth—a process that can take days or weeks depending on jurisdiction.
During this vulnerable window, there’s a real risk of coverage lapses. Without a seamless transition plan, intended parents could face massive medical bills or delays in critical care.
Regional Disparities in Insurance Access
Insurance coverage for surrogacy varies dramatically across geographic regions, reflecting broader differences in healthcare policy, cultural attitudes, and legal frameworks.
United States: A Patchwork System
The U.S. lacks a unified national approach to fertility care. Coverage depends heavily on state laws, employer policies, and individual insurance carriers. States like Massachusetts, Illinois, and New Jersey have made strides in mandating fertility benefits, but others offer no protections whatsoever.
Furthermore, employer-sponsored plans under the Employee Retirement Income Security Act (ERISA) are federally regulated and exempt from state mandates, creating another layer of complexity. Large corporations may choose to offer inclusive fertility benefits as part of competitive employee packages, but small businesses often cannot afford such offerings.
Canada and the UK: Public Healthcare with Private Costs
In Canada, while provincial healthcare covers basic maternity services for surrogates, it does not fund IVF, legal fees, or surrogate compensation. Intended parents must rely on private clinics and out-of-pocket payments, making the process financially burdensome despite having universal healthcare.
Similarly, in the UK, the National Health Service (NHS) provides limited IVF funding, but eligibility criteria are strict, and surrogacy-related treatments are generally excluded. Legal parentage transfer also requires a parental order, adding time and cost to the process.
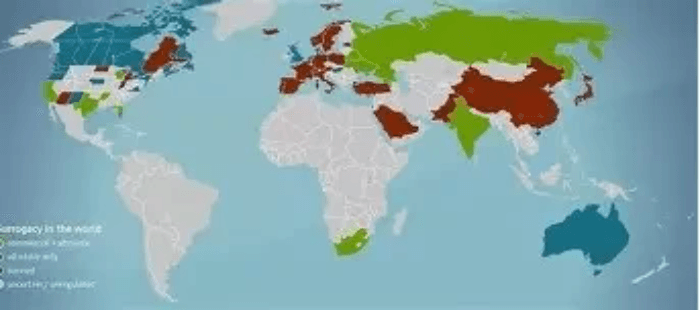
Global Destinations and Ethical Concerns
Some intended parents turn to international surrogacy in countries like Georgia, Ukraine, or Mexico due to lower costs and more flexible regulations. However, these arrangements come with significant risks, including unclear insurance liability, language barriers, and potential exploitation of economically disadvantaged women.
Crucially, international surrogacy often voids domestic insurance coverage entirely. Travel-related complications, emergency evacuations, or cross-border legal disputes are typically not covered, exposing all parties to unforeseen liabilities.
Financial Burden on Intended Parents and Surrogates
The absence of robust insurance coverage translates into substantial financial strain. On average, a single surrogacy journey in the U.S. costs between 130,000 and 180,000. Only a fraction of this is typically reimbursable through insurance.
Intended parents often deplete savings, take second mortgages, or seek loans to cover costs. Meanwhile, surrogates—who undergo physical and emotional risks—are usually compensated via third-party escrow accounts, but their own health risks may not be fully protected. If complications arise postpartum or long-term effects emerge (such as uterine scarring or mental health issues), ongoing care may fall outside policy scope.
Even when insurance nominally covers aspects of the process, administrative hurdles—like prior authorizations, claim denials, and appeals—can delay care and increase stress. A 2023 study published in Fertility and Sterility found that nearly 60% of fertility clinics reported frequent insurance claim rejections for ART procedures involving third-party reproduction.
Legal and Ethical Implications of Insurance Gaps
Beyond financial concerns, inadequate insurance raises serious ethical questions about equity, informed consent, and bodily autonomy.
Informed Consent and Risk Disclosure
Surrogates must provide informed consent before participating in a surrogacy arrangement. However, if insurance coverage is ambiguous or incomplete, can true informed consent be achieved? Many surrogates assume their regular health plan will cover pregnancy-related care, only to discover later that exclusions apply.
Legal contracts often include provisions requiring intended parents to purchase supplemental insurance for the surrogate, but enforcement varies. Without standardized oversight, loopholes persist.
Discrimination and Access Inequality
The high cost of uninsured surrogacy disproportionately affects low- and middle-income individuals, same-sex couples, and single prospective parents. This creates a system where access to surrogacy is effectively tied to wealth, undermining principles of reproductive justice.
Moreover, some insurers use gender identity or marital status as criteria for denying coverage, further marginalizing LGBTQ+ communities. Although the Affordable Care Act prohibits sex-based discrimination, enforcement in fertility contexts remains inconsistent.

Emerging Solutions and Industry Innovations
Despite these challenges, momentum is building toward more inclusive and equitable insurance models.
Specialized Fertility Insurance Products
Companies like LGBTQ+ Family Building Insurance, Progyny, and Carrot Fertility now offer tailored plans that include surrogacy components. These programs bundle services such as IVF, genetic testing, legal consultation, and mental health support into comprehensive packages. Some partner directly with employers to integrate benefits into workplace health plans.
These niche insurers use value-based care models, negotiating discounted rates with networks of clinics and reducing administrative waste. Early data suggests participants experience higher success rates and lower overall costs compared to traditional insurance pathways.
Legislative Advocacy and Policy Reform
Advocacy groups such as RESOLVE: The National Infertility Association and Men Having Babies are pushing for legislative changes to expand insurance mandates. Recent proposals in California and New York aim to require large insurers to cover third-party reproduction services without discriminatory exclusions.
At the federal level, the Access to Family Building Act—if passed—would allow taxpayers to claim a credit for surrogacy-related expenses, similar to existing adoption tax credits. Such measures could significantly reduce financial barriers.
Employer-Led Benefits Expansion
Forward-thinking companies are recognizing fertility benefits as a key component of diversity, equity, and inclusion (DEI) strategies. Tech giants like Apple, Google, and Microsoft already offer up to $100,000 in surrogacy and IVF coverage for employees. As talent competition intensifies, more organizations may follow suit to attract and retain top performers.
This trend not only improves access but also sends a powerful message about corporate commitment to modern family structures.
Recommendations for Stakeholders
To bridge the gaps in surrogacy insurance coverage, coordinated action is needed across multiple fronts:
- For Intended Parents: Research insurance policies thoroughly before beginning the surrogacy process. Consult with specialists who understand fertility law and insurance coding. Consider supplemental policies or membership-based fertility benefit platforms.
- For Surrogates: Ensure your health plan does not contain surrogacy exclusions. Work with agencies that provide transparent guidance on insurance riders and backup coverage options. Seek independent legal counsel before signing any agreement.
- For Healthcare Providers: Advocate for patients by submitting detailed medical necessity documentation. Stay updated on billing codes specific to third-party reproduction (e.g., Z31.43 for encounter for procreation by surrogate). Push for institutional policies supporting equitable care.
- For Policymakers: Expand state and federal mandates to include comprehensive fertility benefits without discriminatory clauses. Fund research on long-term outcomes for surrogates and children born via ART. Harmonize interstate and international regulations to reduce legal fragmentation.
- For Insurers: Re-evaluate outdated definitions of “medical necessity” to reflect advances in reproductive science. Develop standardized surrogacy add-on riders. Partner with fertility networks to control costs and improve outcomes.

Conclusion: Toward a More Equitable Future
Insurance coverage for surrogacy stands at a crossroads. While technological and social progress has made family building through surrogacy more accessible than ever, outdated insurance frameworks threaten to undermine these gains. The current system leaves too many individuals exposed to financial risk, legal uncertainty, and emotional distress.
Addressing the gaps requires a paradigm shift—one that recognizes surrogacy not as a luxury, but as a legitimate form of reproductive healthcare deserving of equitable support. By expanding coverage mandates, fostering innovation in insurance design, and promoting inclusive policies, we can ensure that the dream of parenthood remains within reach for all who seek it.
As awareness grows and advocacy strengthens, the hope is that one day, comprehensive insurance for surrogacy will no longer be the exception—but the standard.
