For many individuals and couples facing fertility challenges, building a family can feel like an uphill journey. Advances in reproductive medicine, however, have opened doors to hopeful paths once considered out of reach. Two of the most discussed and utilized options in modern fertility treatments are Artificial Insemination (AI) and Surrogacy. While both aim to help people become parents, they differ significantly in process, eligibility, emotional considerations, and legal implications. This comprehensive guide explores the distinctions, benefits, and considerations of each method to help you make informed decisions on your journey to parenthood.
What Is Artificial Insemination?
Artificial Insemination (AI) refers to a medical procedure in which sperm is directly inserted into a woman’s reproductive tract to facilitate fertilization. The most common form is Intrauterine Insemination (IUI), where washed and concentrated sperm is placed directly into the uterus around the time of ovulation.
AI is typically recommended for couples or individuals dealing with:
- Mild male factor infertility (low sperm count or motility)
- Unexplained infertility
- Cervical mucus issues
- Use of donor sperm (for single women or same-sex female couples)
- Ejaculation disorders
The process is relatively non-invasive and cost-effective compared to other assisted reproductive technologies (ART). It often involves ovulation induction using fertility medications to increase the chances of success. Success rates vary depending on age, fertility diagnosis, and whether fertility drugs are used, but generally range from 10% to 20% per cycle.
Ideal Candidates for Artificial Insemination:
- Women with at least one open fallopian tube
- Regular ovulation or responsive to ovulation induction
- Sufficient sperm count (either partner or donor)
- No significant uterine abnormalities

What Is Surrogacy?
Surrogacy is a more complex arrangement in which a woman—known as the surrogate or gestational carrier—carries and gives birth to a baby for another person or couple. There are two main types:
- Gestational Surrogacy: The most common and legally preferred form today. In this method, the embryo is created via In Vitro Fertilization (IVF) using the intended parents’ (or donors’) eggs and sperm. The resulting embryo is then transferred to the surrogate’s uterus. The surrogate has no genetic link to the child.
- Traditional Surrogacy: The surrogate is artificially inseminated with the intended father’s (or donor’s) sperm. In this case, the surrogate is the biological mother of the child, as her own egg is used. This method is less common due to complex legal and emotional considerations.
Surrogacy is often pursued by:
- Intended parents with uterine factor infertility (e.g., absence of uterus, scarring, or repeated implantation failure)
- Same-sex male couples
- Single men seeking biological children
- Individuals with medical conditions that make pregnancy life-threatening
The process involves extensive medical screening, psychological evaluation, legal contracts, and coordination between fertility clinics, agencies, and legal professionals. Costs are significantly higher than AI, often ranging from 100,000 to 150,000 in countries like the United States, including medical, legal, and surrogate compensation expenses.
Key Requirements for Surrogacy:
- Healthy gestational carrier (typically aged 21–40, with prior uncomplicated pregnancies)
- IVF cycle to create embryos
- Legal agreements outlining parental rights and responsibilities
- Emotional and financial preparedness

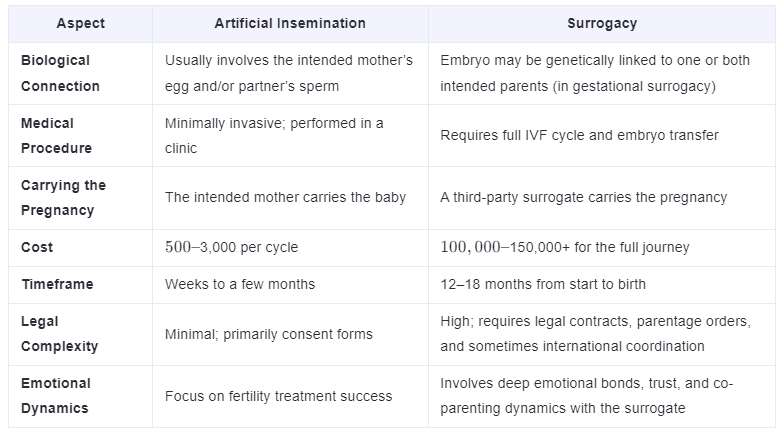
Key Differences Between Artificial Insemination and Surrogacy
While both methods assist in conception, they serve different needs and involve distinct processes. Below is a comparative breakdown:
When Is Artificial Insemination the Right Choice?
AI is often the first-line treatment for couples with mild fertility issues. It’s less invasive, more affordable, and allows the intended mother to experience pregnancy and childbirth. For single women or lesbian couples using donor sperm, AI offers a direct path to biological motherhood.
However, AI may not be suitable if:
- Fallopian tubes are blocked
- There is severe male infertility
- The woman has diminished ovarian reserve
- Previous IUI cycles have failed after 3–6 attempts
In such cases, moving to IVF—which shares embryological groundwork with surrogacy—may be the next step.
When Should You Consider Surrogacy?
Surrogacy becomes a necessary or preferred option when pregnancy is not possible or safe for the intended mother. This includes:
- Hysterectomy or congenital absence of the uterus (Müllerian agenesis)
- Recurrent pregnancy loss due to uterine factors
- Medical conditions such as severe heart disease or cancer that contraindicate pregnancy
- Failed IVF cycles due to implantation issues
For gay male couples and single men, surrogacy is often the only path to having a genetically related child. It allows them to use their own sperm (or donor eggs) and build a biological connection with their child.
Despite its benefits, surrogacy demands significant emotional investment. Building a relationship with the surrogate, navigating legal landscapes, and managing expectations require patience, empathy, and professional support.

Legal and Ethical Considerations
One of the most critical distinctions between AI and surrogacy lies in legal complexity.
Artificial Insemination typically involves straightforward consent forms, especially when using a partner’s sperm. With donor sperm, clinics provide legal waivers relinquishing donor rights. In most jurisdictions, the woman undergoing AI is automatically recognized as the legal mother.
Surrogacy, however, operates in a legal gray area in many countries. Laws vary widely:
- Permitted with restrictions: USA (state-dependent), Canada, Ukraine
- Banned: Germany, France, Italy
- Allowed only altruistically: UK, Australia
Intended parents must secure pre-birth parentage orders or go through adoption processes to be recognized as legal parents. International surrogacy adds layers of immigration, citizenship, and diplomatic challenges.
Ethically, surrogacy raises questions about exploitation, compensation, and autonomy. Reputable agencies and legal frameworks aim to protect all parties, ensuring informed consent, fair compensation, and psychological support.
Emotional and Psychological Aspects
Both AI and surrogacy involve emotional highs and lows, but the nature differs.
With AI, the emotional journey is often internal—closely tied to monthly cycles, hormone fluctuations, and the anxiety of waiting for pregnancy tests. Success may come quickly, or after multiple attempts, requiring resilience.
Surrogacy introduces a third party into the intimate process of conception and birth. While many surrogates form strong, positive relationships with intended parents, boundaries must be carefully managed. Intended parents may experience feelings of detachment from the pregnancy, while surrogates navigate their own emotional attachment to the baby they carry.
Professional counseling is recommended for all parties before, during, and after the surrogacy journey.

Making the Right Choice for Your Family
Choosing between artificial insemination and surrogacy depends on your medical condition, family goals, financial resources, and emotional readiness.
- If you can carry a pregnancy and have viable eggs and sperm (or access to donors), AI may be a practical first step.
- If carrying a pregnancy is not possible or safe, surrogacy offers a viable, though more complex, alternative.
Many fertility clinics offer consultations to evaluate your options. Working with reproductive endocrinologists, counselors, and legal experts ensures you’re fully informed and supported.
Final Thoughts
The journey to parenthood is deeply personal. Whether you pursue Artificial Insemination or Surrogacy, both represent remarkable advances in reproductive science that empower individuals and couples to fulfill their dreams of having a child.
Understanding the differences—medical, emotional, financial, and legal—helps you choose the path that aligns with your circumstances and values. As society evolves and technology advances, these options will continue to expand, offering hope to more people than ever before.
If you’re exploring your fertility options, speak with a qualified reproductive specialist. Your path to parenthood is unique—and entirely possible.
